Volume 5, Issue 1 (June 2019)
Elderly Health Journal 2019, 5(1): 53-57 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghanbari Moghadam A, Mohammadi M, Ardane F, Talebi S, Karbalaee Z. Reliability of Identification of Seniors at Risk Screening Tool in Predicting Functional and Mental Decline in Discharged Elderly Patients. Elderly Health Journal 2019; 5 (1) :53-57
URL: http://ehj.ssu.ac.ir/article-1-128-en.html
URL: http://ehj.ssu.ac.ir/article-1-128-en.html
Akram Ghanbari Moghadam 
 , Mojtaba Mohammadi *
, Mojtaba Mohammadi * 

 , Fateme Ardane
, Fateme Ardane 
 , Shahrbanoo Talebi
, Shahrbanoo Talebi 
 , Zeinab Karbalaee
, Zeinab Karbalaee 


 , Mojtaba Mohammadi *
, Mojtaba Mohammadi * 

 , Fateme Ardane
, Fateme Ardane 
 , Shahrbanoo Talebi
, Shahrbanoo Talebi 
 , Zeinab Karbalaee
, Zeinab Karbalaee 

Dpartment of Health Education and Promotion, Faculty of Health Sciences, Tabriz University of Medical Sciences, Tabriz, Iran , mohammadiuswr@gmail.com
Full-Text [PDF 147 kb]
(950 Downloads)
| Abstract (HTML) (2032 Views)
Article history
Received 10 Oct 2018
Accepted 26 June 2019
A B S T R A C T
Introduction: Emergency wards today are facing with an increasing numbers of older patients. Therefore, it seems important and essential to develop a short screening tool with an acceptable predictive power to identify the seniors being discharged from hospital and mean while are at risk of a decline in physical and mental performance, and thus, facing re-admission emergency wards in hospitals.
Methods: This prospective study was performed on 190 randomly selected elderly people being discharged from emergency centers in Sabzevar city. Data were collected using Identification of Seniors at Risk (ISAR), GHQ-12 and Barthel questionnaires. Descriptive and inferential statistical methods including Pearson correlation coefficient and area under the ROC curve were used for data analysis.
Results: Within the six months period of follow up, the accuracy of ISAR tool for predicting functional and mental performance decline was at a moderate level (AUC = 0.74 , AUC = 0.77 ) but at desirable level for both physical and mental performances, as a whole condition (AUC = 0.84).
Conclusion: ISAR has moderate accuracy to predict the risk of physical or mental decline in elderly people six months after discharge from hospital emergency wards.
Table 1. Screening results of ISAR tool for identifying the elderly at risk of physical and mental decline six months after discharge from the emergency room
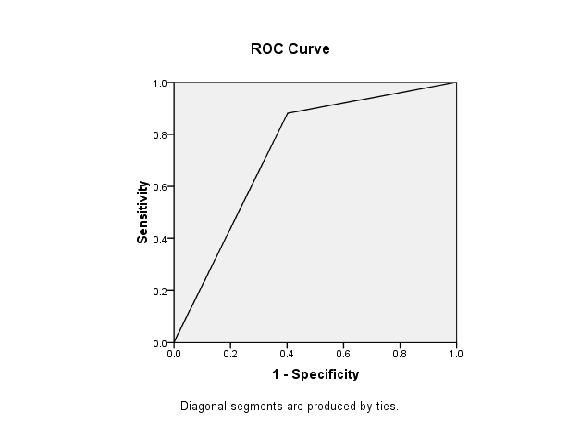
Figure 1. ROC curve for determining the differentiation power (AUC) of (ISAR) Screening Tool in terms of physical performance decline six months after being discharged from an emergency center
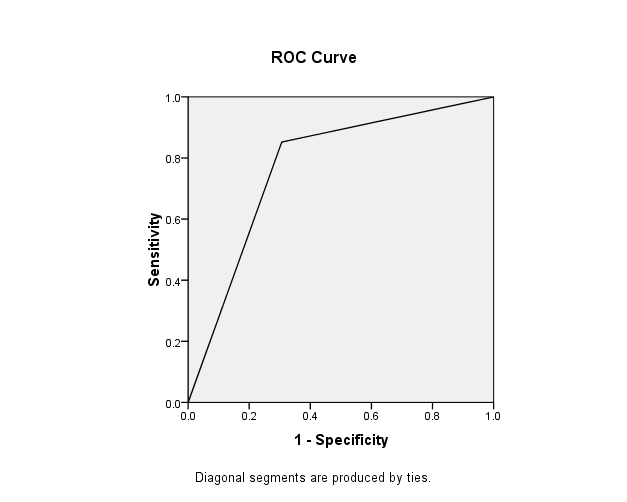
Figure 2. ROC curve for determining the differentiation power (AUC) of (ISAR) Screening Tool in terms of mental performance decline six months after being discharged from an emergency center
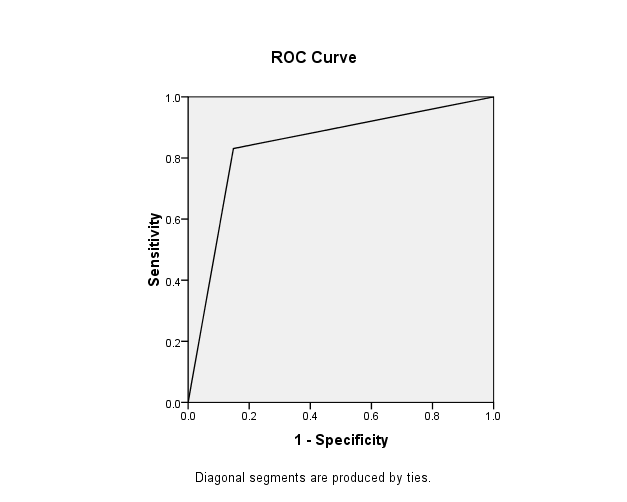
Figure 3. ROC curve for determining the differentiation power (AUC) of (ISAR) Screening Tool in terms of mental and physical performance decline six months after being discharged from an emergency center
Discussion
Full-Text: (824 Views)
Reliability of Identification of Seniors at Risk Screening Tool in Predicting Functional and Mental Decline in Discharged Elderly Patients
Akram Ghanbari Moghaddam 1, Mojtaba Mohammadi *2, 3 , Fateme Ardane 4, Shahrbanoo Talebi 4, Zeinab Karbalaee 5
Akram Ghanbari Moghaddam 1, Mojtaba Mohammadi *2, 3 , Fateme Ardane 4, Shahrbanoo Talebi 4, Zeinab Karbalaee 5
1 .Faculty of Nursing and Midwifery school, Mashhad University of Medical Sciences, Khorasan-e Razavi, Mashhad, Iran
2. Dpartment of Health Education and Promotion, Faculty of Health Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
3. Elderly Research Center, Sabzevar University of Medical Sciences, Khorasan-e Razavi, Sabzevar, Iran
4. Faculty of Nursing and Midwifery, Sabzevar University of Medical Sciences, Khorasan-e Razavi, Sabzevar,Iran
5. Faculty of Nursing, University of Social Welfare & Rehabilitation Sciences, Tehran, Iran
3. Elderly Research Center, Sabzevar University of Medical Sciences, Khorasan-e Razavi, Sabzevar, Iran
4. Faculty of Nursing and Midwifery, Sabzevar University of Medical Sciences, Khorasan-e Razavi, Sabzevar,Iran
5. Faculty of Nursing, University of Social Welfare & Rehabilitation Sciences, Tehran, Iran
Article history
Received 10 Oct 2018
Accepted 26 June 2019
A B S T R A C T
Introduction: Emergency wards today are facing with an increasing numbers of older patients. Therefore, it seems important and essential to develop a short screening tool with an acceptable predictive power to identify the seniors being discharged from hospital and mean while are at risk of a decline in physical and mental performance, and thus, facing re-admission emergency wards in hospitals.
Methods: This prospective study was performed on 190 randomly selected elderly people being discharged from emergency centers in Sabzevar city. Data were collected using Identification of Seniors at Risk (ISAR), GHQ-12 and Barthel questionnaires. Descriptive and inferential statistical methods including Pearson correlation coefficient and area under the ROC curve were used for data analysis.
Results: Within the six months period of follow up, the accuracy of ISAR tool for predicting functional and mental performance decline was at a moderate level (AUC = 0.74 , AUC = 0.77 ) but at desirable level for both physical and mental performances, as a whole condition (AUC = 0.84).
Conclusion: ISAR has moderate accuracy to predict the risk of physical or mental decline in elderly people six months after discharge from hospital emergency wards.
Keywords: Aged, Emergencies, Seniors at Risk
Copyright © 2019 Elderly Health Journal. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cite.
Introduction
Emergency centers are primary providers of urgent care services for major users (1, 2). There have been some reports about re-admission of recently discharged elderlies to emergency centers (3) with some degree of decline in physical and mental health status for the same reasons (1). The seniors may then have other specific and varying needs that are usually neglected by emergency departments because they often focus their special attention on the particular problem that the elderly has referred (4). Seniors may likely to be at an increased risk of re-admission to these centers following discharge. Research has shown that within one month after the discharge, 10% of the elderly discharged from the emergency wards were being readmitted, 24% after 3 months and 44% after 6 months (5, 6). Therefore, the routine assessment of the elderly in emergency centers and the ability of specialists to quickly and appropriately identify the most vulnerable older people can potentially improve the status of the present readmission system of older people to health centers (1). The long-term outcomes of screening for the elderly and intervention based on it, will gradually contribute to an increase in the referrals of elderly people at risk to the primary caregivers of health using a preventive approach (1). Timely and proper delivery of appropriate care can significantly help reduce mortality rate and even physical and mental disabilities. To consider this issue is so important that the application of screening for the identification of seniors at risk may easily help treat one in every three elderly patients (7). The Identification of Seniors at Risk (ISAR) is one of the most commonly used and best-validated screening tools which provide immediate and rapid administration and its validity and credibility to anticipate some of the negative consequences in the elderly have been identified and confirmed in a number of studies in various countries (8-11), as well as widely used in emergency rooms (12). ISAR instrument items measure common problems including physical performance decline, cognitive dysfunction, numbers of medication used, visual impairment, and numbers of hospital admissions (13). However, it is noticeable that the predictive power of the widely used tool, ISAR has yielded different values in different countries. These discrepancies can be attributable to the health services available in these countries and research samples (14). In order to examine the feasibility of using this tool in Iran, we need to evaluate its appropriate predictive power in our society. In pursuit of this goal, we sought to assess the predictive power of the physical and mental performance of this tool among the elderly in Iran.
Method
Participants and Procedures
In this prospective study, the statistical population consisted of elderly people discharged from emergency wards in Sabzevar. One hundred and ninety older people were randomly selected and filled out ISAR, GHQ-12 and Barthel questionnaires along with demographic information questionnaire. The inclusion criteria were: over 60 years of age and discharge to home after receiving emergency treatment. The exclusion criteria were: reluctance to answer questions and lack of cooperation in the follow-up period of the study. With the help of interviewers trained by the research team, the questionnaires were completed by observing and interviewing with eligible elderly or his/her companion (family members or care givers in the event of a cognitive impairment or temporary loss of alertness) at the Emergency wards of Emdad and Vasei Hospitals in Sabzevar, Iran. Six months after the discharge, information on physical and mental status was collected via telephone call or face-to-face interview.
Instruments
ISAR Screening Tool has 6 items and measure common problems including physical performance decline, cognitive dysfunction, numbers of medication used, visual impairment, and numbers of hospital admissions. Each item is answered with "yes" or "no" response and older people had a gain score between 0 and 6. Subjects with a score of 2 or more are more susceptible or "at risk." The reliability of the tool was calculated 0.78 using test-retest method (13).
Barthel Index was used to evaluate physical performance. It was designed by Mahoney and Barthel to measure functional abilities before and after treatment (12). The reliability of the Persian version of the Barthel and its validity is reported 0.9 (13). The Barthel instrument is a worldwide popular and standard indicator which has been widely used in many similar studies (6, 12, 13). The Barthel index has 10 components including eating, bathing, make-up, stool and urine control, using the toilet or tub, moving from bed to chair and moving up and down the stairs. Based on Barthel et al., classification, the score 0-59 is unable, 60-84 have less independency, 85-94 have medium independency, 95-99 have relative independency, and 100 are independent (13).
General Health Questionnaire (GHQ) was used to measure the mental health status which was developed by Goldberg in 1972 to identify mental disorders in various centers and environments (16). The questionnaire is widely used both in Iran and other countries (16-18). The most commonly used scoring method in GHQ questionnaire is Likert scale. Each item of the GHQ was rated on a four-point scale Likert scoring system (0-1-2-3). The maximum score for the GHQ-12 questionnaire is 36 (18). In Iran, the Cronbach's alpha coefficient was estimated to be 0.87 showing that the Iranian version of GHQ-12 had an acceptable reliability and validity to measure mental health status among the Iranian people (17-18).
Ethical considerations
The participants were ensured that all information provided would be kept confidential and all the concerned authorities can benefit from the results of the research, if they wish. The study protocol was approved as a master's thesis at the University of Social Welfare and Rehabilitation Sciences of Tehran with ethics code (ir.uswr.rec.1394.125).
Statistical analysis
Data were analyzed viaSPSS software using descriptive and inferential statistical methods such as Pearson correlation coefficient and area under the ROC curve. Since in a number of studies regarding the estimation of predictive and diagnostic power of screening tools, area under the ROC curve has been the dominant used tool, then we firstly chose to draw area under the ROC curve and the AUC level for each of the negative consequences of the study. The values of AUC are interpreted as follows: 0.90 to 1, high differentiation power, 0.88 to 0.89 good differentiation powers, 0.70 to 0.79 average differentiation powers, 0.69 to 60/0 weak differentiation powers and a value of 59/0 to 50/0 had no differentiation power (19).
Results
The mean age of participants was 72 ± 9.5 years. Ninty six percent of the elderly discharged from emergency centers had at least one chronic disease. Forty six percent of the elderly named their spouse as their primary caregiver and 74% of male elderly are cared for at home by their wife. Married girls (13%) and boys (12%) were responsible for the care of their parents, respectively. Approximately 16% of the elderly had no one to take care of them and 52% of older people were supported in care home at night. In 11 cases, care was provided daily at home. The screening results of ISAR tool for identifying the elderly at risk of physical and mental decline after discharge from the emergency centers are presented in table 1.
The ROC curves and the AUC level for each of the physical and mental performance decline, and both of them, six months after being discharged from an emergency center are shown in Figures 1 to 3.
Method
Participants and Procedures
In this prospective study, the statistical population consisted of elderly people discharged from emergency wards in Sabzevar. One hundred and ninety older people were randomly selected and filled out ISAR, GHQ-12 and Barthel questionnaires along with demographic information questionnaire. The inclusion criteria were: over 60 years of age and discharge to home after receiving emergency treatment. The exclusion criteria were: reluctance to answer questions and lack of cooperation in the follow-up period of the study. With the help of interviewers trained by the research team, the questionnaires were completed by observing and interviewing with eligible elderly or his/her companion (family members or care givers in the event of a cognitive impairment or temporary loss of alertness) at the Emergency wards of Emdad and Vasei Hospitals in Sabzevar, Iran. Six months after the discharge, information on physical and mental status was collected via telephone call or face-to-face interview.
Instruments
ISAR Screening Tool has 6 items and measure common problems including physical performance decline, cognitive dysfunction, numbers of medication used, visual impairment, and numbers of hospital admissions. Each item is answered with "yes" or "no" response and older people had a gain score between 0 and 6. Subjects with a score of 2 or more are more susceptible or "at risk." The reliability of the tool was calculated 0.78 using test-retest method (13).
Barthel Index was used to evaluate physical performance. It was designed by Mahoney and Barthel to measure functional abilities before and after treatment (12). The reliability of the Persian version of the Barthel and its validity is reported 0.9 (13). The Barthel instrument is a worldwide popular and standard indicator which has been widely used in many similar studies (6, 12, 13). The Barthel index has 10 components including eating, bathing, make-up, stool and urine control, using the toilet or tub, moving from bed to chair and moving up and down the stairs. Based on Barthel et al., classification, the score 0-59 is unable, 60-84 have less independency, 85-94 have medium independency, 95-99 have relative independency, and 100 are independent (13).
General Health Questionnaire (GHQ) was used to measure the mental health status which was developed by Goldberg in 1972 to identify mental disorders in various centers and environments (16). The questionnaire is widely used both in Iran and other countries (16-18). The most commonly used scoring method in GHQ questionnaire is Likert scale. Each item of the GHQ was rated on a four-point scale Likert scoring system (0-1-2-3). The maximum score for the GHQ-12 questionnaire is 36 (18). In Iran, the Cronbach's alpha coefficient was estimated to be 0.87 showing that the Iranian version of GHQ-12 had an acceptable reliability and validity to measure mental health status among the Iranian people (17-18).
Ethical considerations
The participants were ensured that all information provided would be kept confidential and all the concerned authorities can benefit from the results of the research, if they wish. The study protocol was approved as a master's thesis at the University of Social Welfare and Rehabilitation Sciences of Tehran with ethics code (ir.uswr.rec.1394.125).
Statistical analysis
Data were analyzed via
Results
The mean age of participants was 72 ± 9.5 years. Ninty six percent of the elderly discharged from emergency centers had at least one chronic disease. Forty six percent of the elderly named their spouse as their primary caregiver and 74% of male elderly are cared for at home by their wife. Married girls (13%) and boys (12%) were responsible for the care of their parents, respectively. Approximately 16% of the elderly had no one to take care of them and 52% of older people were supported in care home at night. In 11 cases, care was provided daily at home. The screening results of ISAR tool for identifying the elderly at risk of physical and mental decline after discharge from the emergency centers are presented in table 1.
The ROC curves and the AUC level for each of the physical and mental performance decline, and both of them, six months after being discharged from an emergency center are shown in Figures 1 to 3.
Table 1. Screening results of ISAR tool for identifying the elderly at risk of physical and mental decline six months after discharge from the emergency room
| Screening results for ISAR tool | Number | Real status six months after discharge from the emergency room | Physical performance decline | Mental performance decline | Physical or mental performance decline |
| At risk in terms of tool (positive) | 121 | Being at risk (real positive) | 93 | 115 | 136 |
| No risk based on the (negative) | 69 | Not being at risk (real and negative) | 98 | 76 | 55 |
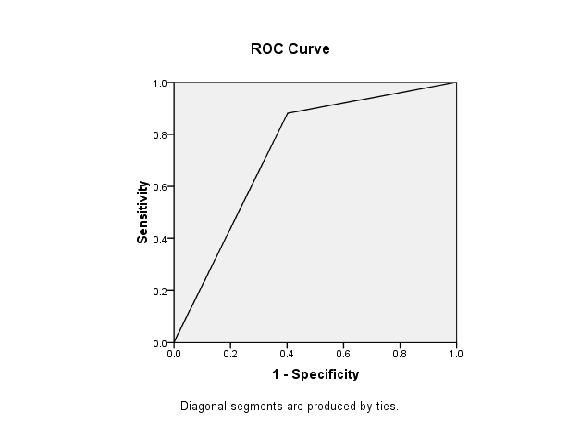
Figure 1. ROC curve for determining the differentiation power (AUC) of (ISAR) Screening Tool in terms of physical performance decline six months after being discharged from an emergency center
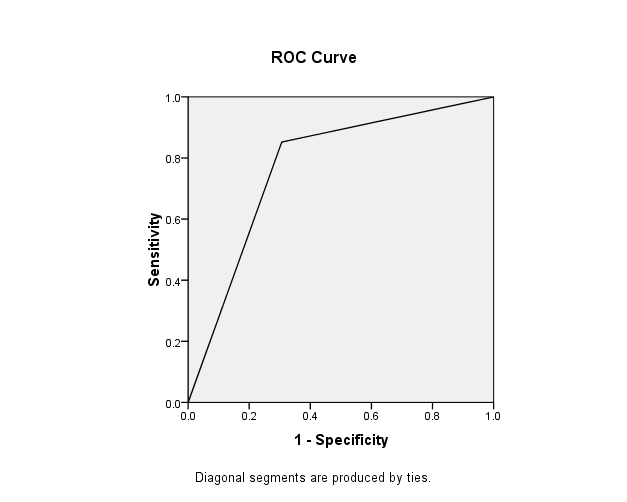
Figure 2. ROC curve for determining the differentiation power (AUC) of (ISAR) Screening Tool in terms of mental performance decline six months after being discharged from an emergency center
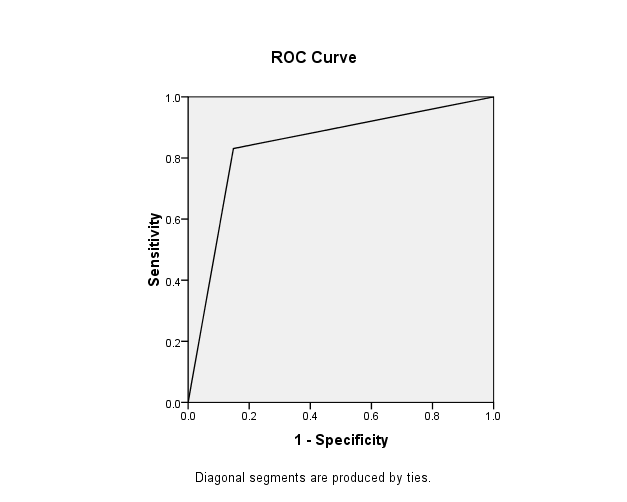
Figure 3. ROC curve for determining the differentiation power (AUC) of (ISAR) Screening Tool in terms of mental and physical performance decline six months after being discharged from an emergency center
Discussion
It was found that the accuracy of ISAR tool for predicting physical and mental performance decline, six months after the discharge of seniors from the emergency wards, was moderate in Iran (AUC 0.74 -0.84). However, the results, the accuracy of ISAR tool for prediction of both the physical and mental performance declines among the elderly, as a whole condition, 6 month after discharge has been evaluated at a desirable and "good" level. The findings of other studies by Salvi et al. (7), Hoogerduijn et al. (8) and Moons et al. (5) also show that the accuracy of the tool for predicting re-admission in emergency situations was at low to moderate levels (AUC = 0.65 - 0.70), which is consistent with the results of the present study . It seems that in these studies, the criterion of returning the elderly to emergency wards as the only predicted negative consequence after discharge, has contributed to the weak or moderate power of this tool. Our findings also support the contributing role of the criteria. Therefore, the results indicate that the ISAR tool has more favorable accuracy in predicting more than one negative outcome. The study suggests that the elderly who are considered to be at risk by this tool are either physically or psychologically impaired, but this does not mean that the elderly is necessarily subject to physical return to the emergency room. Since our study showed that physical or mental performance decline is well thought out by the ISAR tool, it is suggested that this tool be used to prevent the development of physical and mental disabilities in the elderly. Overall, it seems that according to the current study, the ISAR tool has a medium-to-high predictive accuracy for identifying the elderly at risk of physical and mental decline.
Conclusion
Based on the results, the ISAR tool can be considered as one of the valid screening tools for identifying the elderly at risk of physical and psychological decline after discharge from emergency wards in the Iranian senior's assessment list.
Conflict of interest
Authors declare no potential conflict of interest with respect to the authorship and/or publication of this article.
Acknowledgments
The professors of the University of Welfare and Rehabilitation Sciences of Tehran, the officials and employees of the Emergency Department of Emdad and Vasei Hospital in Sabzevar and the colleagues who were inquiring, were able to carry out this research with their sincere cooperation are appreciated.
Authors' contributions
Mojtaba Mohammadi, Fateme ardane and Akram Ghanbari Moghaddam h: Design and management of the study. Mojtaba Mohammadi, Shahrbanoo Talebi, Fateme Ardaneh and Zeinab Karbalaee: Analysis,writing and rewriting.
All the author have read the final manuscript and approved that.
References
Conclusion
Based on the results, the ISAR tool can be considered as one of the valid screening tools for identifying the elderly at risk of physical and psychological decline after discharge from emergency wards in the Iranian senior's assessment list.
Conflict of interest
Authors declare no potential conflict of interest with respect to the authorship and/or publication of this article.
Acknowledgments
The professors of the University of Welfare and Rehabilitation Sciences of Tehran, the officials and employees of the Emergency Department of Emdad and Vasei Hospital in Sabzevar and the colleagues who were inquiring, were able to carry out this research with their sincere cooperation are appreciated.
Authors' contributions
Mojtaba Mohammadi, Fateme ardane and Akram Ghanbari Moghaddam h: Design and management of the study. Mojtaba Mohammadi, Shahrbanoo Talebi, Fateme Ardaneh and Zeinab Karbalaee: Analysis,writing and rewriting.
All the author have read the final manuscript and approved that.
References
- Aminzadeh F, Dalziel Wb. Older adults in the emergency department: a systematic review of pattern of use, adverse outcomes and effectiveness of interventions. Annals of Emergency Medicine. 2002; 39(3): 238-247.
- Di Bari M, Salvi F, Roberts AT, Balzi D, Lorenzetti B, Morichi V, et al. Prognostic stratification of elderly patients in the emergency department: a comparison between the ‘identification of seniors at risk’ and the "Silver Code". The Journals of Gerontology. 2012; 67(5): 544–50.
- Mccusker J, Verdon J. Do geriatric interventions reduce emergency department visits? a systematic review. The Journals of Gerontology.Series A, Biological Sciences and Medical Sciences. 2006; 61(1): 53–62.
- Salvi F, Morichi V, Grilli A, Lancioni L, Spazzafumo L, Polonara S, et al. Screening for frailty in elderly emergency department patients by using the identification of seniors at risk (ISAR). The Journal of Nutrition, Health & Aging. 2012 Apr; 16(4): 313-8.
- Moons P, De Ridder K, Geyskens K, Sabbe M, Braes T, Flamaing J, et al. Screening for risk of readmission of patients aged 65 years and above after the discharge from the emergency department: predictive value of four instruments. European Journal of Emergency Medicine: Official Journal of the European Society for Emergency Medicine. 2007; 14(6):315–23.
- Buurman BM, Van Den Berg W, Korevaar JC, Milisen K, De Haan RJ, De Rooij SE. Risk for poor outcomes in older patients discharged from an emergency department: feasibility of four screening instruments. European Journal of Emergency Medicine: Official Journal of the European Society for Emergency Medicine. 2011; 18(4): 215–20.
- Salvi F, Morichi V, Grilli A, Spazzafumo L, Giorgi R, Polonara S, et al. Predictive validity of the Identification of Seniors At Risk (ISAR) screening tool in elderly patients presenting to two Italian emergency departments. Aging Clinical and Experimental Research. 2009; 21(1): 69-75.
- Mohammadi M, Ghanbari Moghaddam A, Pourrahimi A, Mohammadzadeh M, Mohammadi Shahboulaghi F. psychometric properties of the farsi version of isar used in iranian emergency centers. Pharmacophore. 2017, 8(6S): 1-6.
- Samaras N, Chevalley T, Samaras D, Gold G. Older patients in the emergency department: a review. Annals of Emergency Medicine. 2010; 56(3): 261-9.
- McCusker J, Jacobs P, Dendukuri N, Latimer E, Tousignant P, Verdon J. Cost-effectiveness of a brief 2-stage emergency department intervention for high risk elders: results of a quasirandomized controlled trial. Annals of Emergency Medicine. 2003; 41(1): 45–56
- Edmans J, Bradshaw L, Gladman JRF, Franklin M, Berdunov V, Elliott R. The identification of seniors at risk (ISAR) score to predict clinical outcomes and health service costs in older people discharged from UK acute medical units .Age And Ageing 2013; 42(6): 747–53 .
- Mahoney FI, Barthel D. Functional evaluation: the barthel index. Maryland State Medical Journal. 1965; 14: 56-61.
- Tagharrobi Z, Sharifi KH, Sooky Z .Psychometric evaluation of the short forms of barthel index in the elderly residing in nursing home. Journal of Paramedical Science and Rehabilitation. 2013; 2(1): 26-38. [Persian]
- Hoogerduijn JG, Schuurmans MJ, Korevaar JC, Buurman BM, De Rooij SE. Identification of older hospitalised patients at risk for functional decline, a study to compare the predictive values of three screening instruments. Journal of Clinical Nursing. 2010; 19(9-10): 1219-25.
- McCusker J, Cardin S, Bellavance F, Belzile É. Return to the emergency department among elders: Patterns and predictors. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine. 2000; 7(3): 249-59.
- Goldberg D, Williams P. A users guide to the General Health Questionnaire.Windsor, Berks: NFER-Nelson; 1988.
- Taghavi M. Validity and reliability of the general health questionnaire (ghq-28) in college students of Shiraz universi1y. Journal of Psychology. 2002; 5(4); 381-398. [Persian]
- Malakooti SK, Mirabzadeh A, Fathollahi P, Salavati M, Kahali SH, Afhamebrahimi A, et al. Reliability ,validity and factor analysis of the GHQ-28 in Iranian elderly. Salmand, Iranian Journal of Aging. 2006; 1(1): 11-21. [Persian]
- Sharifi HP. Principles of psychometric and psychological testing. Tehran: Roshd publisher; 2011.
Type of Study: Research |
Subject:
Special
Received: 2018/10/25 | Accepted: 2019/06/26 | Published: 2019/06/27
Received: 2018/10/25 | Accepted: 2019/06/26 | Published: 2019/06/27
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |