Volume 6, Issue 2 (December 2020)
Elderly Health Journal 2020, 6(2): 122-130 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rebecca D, Eicher C, Ferizaj D. Evaluation of a Music Intervention on Well-being and Behavior of People with Dementia Using Dementia Care Mapping. Elderly Health Journal 2020; 6 (2) :122-130
URL: http://ehj.ssu.ac.ir/article-1-196-en.html
URL: http://ehj.ssu.ac.ir/article-1-196-en.html
Geriatrics Research Group, Charité – Universitätsmedizin Berlin, Berlin, Germany , rebecca.dahms@charite.de
Full-Text [PDF 677 kb]
(615 Downloads)
| Abstract (HTML) (1846 Views)
.png)
Table 1. Overview of the music interventions
Note. Music therapy and music-based interventions were not offered on Sundays
* If the music disturbed the PwD during meals, they had the possibility to eat in their room at any time.
** The PwD had the choice of turning off the radio themselves or having it turned off.
Table 2. List of well-and ill-being values (WIB)
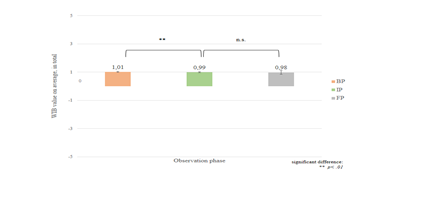
Figure 2. WIB value on average, in total
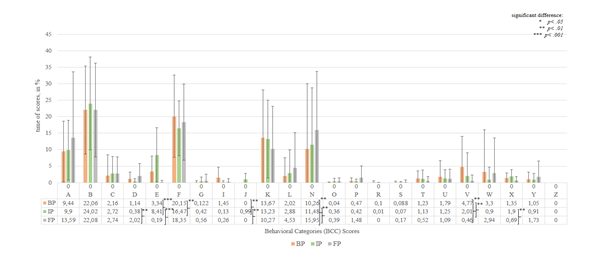
Figure 3. BCC time scores in %
Full-Text: (987 Views)
Evaluation of a Music Intervention on Well-being and Behavior of People with Dementia Using Dementia Care Mapping
Rebecca Dahms *1 , Cornelia Eicher 1, Drin Ferizaj 1
Article history
Received 16 Jul 2020
Accepted 5 Oct 2020
A B S T R A C T
Introduction: Dementia Care Mapping (DCM) was originally developed as an observation tool to examine person-centered care in long-term care facilities and to evaluate the quality of life and well-being of people with dementia (PwD). However, the effects of a music intervention using this tool have not been investigated so far. This leads to the following research question: How does a music intervention which involves music therapy and other music-based interventions affect the observed well-being and behavior of PwD living in nursing homes?
Methods: In this 14-week, non-controlled music intervention study, data from 30 PwD aged between 52 and 97 (M = 81.4 years) were analyzed. DCM coding involves continuous observation for five hours on four days in the baseline and intervention phase. In the follow-up phase PwD were mapped on two days for five hours. The DCM method were used to measure well-being and certain behaviors of PwD.
Results: The well-being during the observation remained almost constant and corresponds to a neutral state of affect and focused contact, with no indication of positive or negative sensations. Significant improvements in certain behaviors were observed in the course from baseline to intervention phase. For example, it was shown that physical activities of the participants, such as (instructed) sports exercises, strengthening or physically challenging exercises in the intervention phase were significantly higher (M = 0.99, SD = 1.82) than at baseline phase (M = 0.00, SD = 0.00) (z = -2.37, p = .02, n = 26). Similar results were shown for expressive/creative activities or work-related activities (e.g. washing dishes).
Conclusion: In summary, it can be stated that music interventions can promote communication and movement. However, musical stimulation is not one of the essential components of improving behavioral and psychological symptoms or well-being for PwD in nursing homes.
Keywords: Dementia, Music Therapy, Behavioral Symptoms, Well-Being, Dementia Care Mapping
Copyright © 2020 Elderly Health Journal. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cite.
Rebecca Dahms *1 , Cornelia Eicher 1, Drin Ferizaj 1
- Geriatrics Research Group, Charité – Universitätsmedizin Berlin, Berlin, Germany
Article history
Received 16 Jul 2020
Accepted 5 Oct 2020
A B S T R A C T
Introduction: Dementia Care Mapping (DCM) was originally developed as an observation tool to examine person-centered care in long-term care facilities and to evaluate the quality of life and well-being of people with dementia (PwD). However, the effects of a music intervention using this tool have not been investigated so far. This leads to the following research question: How does a music intervention which involves music therapy and other music-based interventions affect the observed well-being and behavior of PwD living in nursing homes?
Methods: In this 14-week, non-controlled music intervention study, data from 30 PwD aged between 52 and 97 (M = 81.4 years) were analyzed. DCM coding involves continuous observation for five hours on four days in the baseline and intervention phase. In the follow-up phase PwD were mapped on two days for five hours. The DCM method were used to measure well-being and certain behaviors of PwD.
Results: The well-being during the observation remained almost constant and corresponds to a neutral state of affect and focused contact, with no indication of positive or negative sensations. Significant improvements in certain behaviors were observed in the course from baseline to intervention phase. For example, it was shown that physical activities of the participants, such as (instructed) sports exercises, strengthening or physically challenging exercises in the intervention phase were significantly higher (M = 0.99, SD = 1.82) than at baseline phase (M = 0.00, SD = 0.00) (z = -2.37, p = .02, n = 26). Similar results were shown for expressive/creative activities or work-related activities (e.g. washing dishes).
Conclusion: In summary, it can be stated that music interventions can promote communication and movement. However, musical stimulation is not one of the essential components of improving behavioral and psychological symptoms or well-being for PwD in nursing homes.
Keywords: Dementia, Music Therapy, Behavioral Symptoms, Well-Being, Dementia Care Mapping
Copyright © 2020 Elderly Health Journal. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cite.
Introduction
Worldwide, approximately 50 million people currently suffer from dementia and this number will increase to more than 100 million by 2050 (1). Dementia is defined as a syndrome associated with a disruption of higher cortical functions (such as memory, thinking, judgment, speech, etc.) and impaired everyday functions (2). While disorders of consciousness are not present, disorders of emotional control, social behavior or motivation occasionally accompany the appearance (3).
As dementia progresses and its severity increases, the complexity of care needs equally increases, making in-home care no longer possible. As a consequence, people with dementia (PwD) often have to move into a nursing home (4,5) which means the proportion of PwD in inpatient care facilities is growing steadily. The World Alzheimer Report from 2013 has reported four-fifths of older people in nursing homes to suffer from dementia (6). In addition, several studies have shown that PwD in nursing homes with a prevalence rate of at least 50% exhibit dementia-associated behavioral and psychological symptoms of dementia (BPSD) such as agitation, apathy, depression, disorientation, day-night rhythm disturbance and other co-existing diseases such as Parkinson's disease, which can promote dementia (7–10). These symptoms are most common, difficult to manage and have a negative impact on the functional status (limited mobility), quality of life and well-being of PwD.
Since there are no treatments currently available to cure dementia, drug therapy is the predominant treatment for PwD, which also applies to long-term care facilities (11). In addition to drug-based dementia therapy, however, non-pharmacological therapeutic interventions such as music therapy are also recommended for psychosomatic and psychotherapeutic treatment. Music therapy or music-based interventions (supported by technology) can be used through all stages of dementia, especially in cases of severe dementia (12). Nevertheless, music therapy and music-based interventions can function as a medium for PwD to engage more physical (13) and cognitive actively with their environment as well as to improve BPSD (14, 15). Music can also assist in expressing their feelings and emotions better (16, 17). Furthermore, music therapy can help improve perceived quality of life and well-being (18, 19). Recent studies of the music and memory concept have shown that this music should be tailored to the personal needs, i.e. the musical preferences, in order to achieve the physiological, psychological and emotional impact for PwD (17, 20-23).
In addition to music therapy as a non-drug therapy method, further psychosocial interventions in nursing practice are recommended, which on the one hand should contribute to the improvement of challenging behaviors an on the other hand should support and optimize person-centered care on the caregivers' perspective, including Dementia Care Mapping (DCM) (24–27).
However, the effects of music therapy and music-based interventions (including technology-based interventions) based on musical preferences on PwD in nursing homes as observed by the DCM are still unknown. The following research question therefore arises: How does a music intervention involving music therapy and music-based interventions (using technology) affect the observed behavior and well-being of PwD?
Methods
Research design
The researcher (certified study director and study staff according to the international Good Clinical Practice guidelines) conducted a non-controlled music intervention study over a period of 14 weeks in three nursing homes with PwD and their caregivers.
Data collection
The study was divided into four study visits (see figure 1). In this paper only the results from the Demantia Care Mapping (DCM) observations of PwD were considered.
Due to the limited ability of the PwD, prior to the start of the study, the caregivers of PwD were informed about the course and content of the study by a written and oral study information. The inclusion criteria for PwD were a clinically diagnosed dementia and they had to be able to mobilize freely to participate in the music interventions independently of others. The exclusion criteria was a lack of verbal expression. After that, all caregivers gave written informed consent. All questionnaires were external assessment questionnaires. The selection of the PwD, who took part in the study was made by the caregivers in the nursing homes.
Sociodemographic data were collected in the baseline phase (BP). In addition (among other assessments) DCM (24, 25) was conducted at each time of the study.
The following music interventions were provided during the intervention phase (IP) (see table 1):
Group music therapy
Individual music therapy
Group music with movements
Music program via TV in a common room
Personal radio in the residents’ own room
Standardized background music
As dementia progresses and its severity increases, the complexity of care needs equally increases, making in-home care no longer possible. As a consequence, people with dementia (PwD) often have to move into a nursing home (4,5) which means the proportion of PwD in inpatient care facilities is growing steadily. The World Alzheimer Report from 2013 has reported four-fifths of older people in nursing homes to suffer from dementia (6). In addition, several studies have shown that PwD in nursing homes with a prevalence rate of at least 50% exhibit dementia-associated behavioral and psychological symptoms of dementia (BPSD) such as agitation, apathy, depression, disorientation, day-night rhythm disturbance and other co-existing diseases such as Parkinson's disease, which can promote dementia (7–10). These symptoms are most common, difficult to manage and have a negative impact on the functional status (limited mobility), quality of life and well-being of PwD.
Since there are no treatments currently available to cure dementia, drug therapy is the predominant treatment for PwD, which also applies to long-term care facilities (11). In addition to drug-based dementia therapy, however, non-pharmacological therapeutic interventions such as music therapy are also recommended for psychosomatic and psychotherapeutic treatment. Music therapy or music-based interventions (supported by technology) can be used through all stages of dementia, especially in cases of severe dementia (12). Nevertheless, music therapy and music-based interventions can function as a medium for PwD to engage more physical (13) and cognitive actively with their environment as well as to improve BPSD (14, 15). Music can also assist in expressing their feelings and emotions better (16, 17). Furthermore, music therapy can help improve perceived quality of life and well-being (18, 19). Recent studies of the music and memory concept have shown that this music should be tailored to the personal needs, i.e. the musical preferences, in order to achieve the physiological, psychological and emotional impact for PwD (17, 20-23).
In addition to music therapy as a non-drug therapy method, further psychosocial interventions in nursing practice are recommended, which on the one hand should contribute to the improvement of challenging behaviors an on the other hand should support and optimize person-centered care on the caregivers' perspective, including Dementia Care Mapping (DCM) (24–27).
However, the effects of music therapy and music-based interventions (including technology-based interventions) based on musical preferences on PwD in nursing homes as observed by the DCM are still unknown. The following research question therefore arises: How does a music intervention involving music therapy and music-based interventions (using technology) affect the observed behavior and well-being of PwD?
Methods
Research design
The researcher (certified study director and study staff according to the international Good Clinical Practice guidelines) conducted a non-controlled music intervention study over a period of 14 weeks in three nursing homes with PwD and their caregivers.
Data collection
The study was divided into four study visits (see figure 1). In this paper only the results from the Demantia Care Mapping (DCM) observations of PwD were considered.
Due to the limited ability of the PwD, prior to the start of the study, the caregivers of PwD were informed about the course and content of the study by a written and oral study information. The inclusion criteria for PwD were a clinically diagnosed dementia and they had to be able to mobilize freely to participate in the music interventions independently of others. The exclusion criteria was a lack of verbal expression. After that, all caregivers gave written informed consent. All questionnaires were external assessment questionnaires. The selection of the PwD, who took part in the study was made by the caregivers in the nursing homes.
Sociodemographic data were collected in the baseline phase (BP). In addition (among other assessments) DCM (24, 25) was conducted at each time of the study.
The following music interventions were provided during the intervention phase (IP) (see table 1):
Group music therapy
Individual music therapy
Group music with movements
Music program via TV in a common room
Personal radio in the residents’ own room
Standardized background music
.png)
Figure 1. Data collection
All music therapists had experience in the therapeutic work with PwD. The provided music of the individual and group music therapy was improvised music, which was mainly played by guitar, but also by other instruments (e.g. singing bowls, percussion). The songs of the music-based interventions were selected on the recommendation of the professional caregivers and relatives. The playing speed was adjusted (slowing down) for all music-based interventions prior to the study. Furthermore, the volume was always adjusted so that the majority of PwD could hear it. The impact of individual interventions on PwD is not part of this paper.
Instrumentation
The general DCM observation method: The DCM is an observation and evaluation tool which is used to optimize the overall care for PwD. It can be used both as an instrument for developing a person-centered care practice and as a research instrument. Based on an intensive, real-time observation of several hours by one or more observers, the so-called "mappers", the behavior of five to a maximum of eight PwD is recorded simultaneously over a period of four to a maximum of eight hours. The observed behavior is classified and coded into different behavior categories in a time interval of five minutes. The observation takes place exclusively in public spaces and common areas of the care institution (24, 25, 28).
The DCM observation method in the study: Using the DCM method, each resident in the study was observed for five hours in the baseline phase on four days and at the beginning of the intervention phase in week 3 and 4, as well as at the end of the intervention phase in week 7 and 8 on two days. During the last phase (week 13 and 14), the follow-up phase, PwD were mapped again on two days for five hours in the last two weeks.
To ensure an accurate observation, the mapper divided the residents into groups. In two of the three nursing homes, group sizes of five PwD per observation unit (five hours) were selected (a total of two groups with five PwD). In the third care institution, a group size of six PwD per observation unit (five hours) was chosen for the DCM (a total of two groups with 6 PwD). Two PwD had to be excluded due to their death shortly after the start of the study. PwD observations were preferred on days when music interventions took place (e.g. preferred group music therapy and individual music therapy) to understand the effects on well-being and behaviour more effectively.
Up to two different types of information were encoded during observation of the residents: (1) well-being or ill-being (WIB) and (2) Behavior Category Codes (BCC) observed during interactions between caregivers and residents. In terms of well-being and ill-being the mapper gave a WIB value (-5, -3, -1, +1, +3, +5) (see table 2) for each five-minute observation, depending on the signs of well-being shown by the PwD during this five-minute period.
The behavior of the PwD was also coded every five minutes. The DCM tool provides a template for this, covering 23 categories that reflect the range of behaviors that PwD living in institutional settings can display. These categories included behaviors that indicate both an active engagement with the environment (e.g. communication, leisure) and a lack of involvement in that environment (e.g. sleep, non-involvement) (see Table 3). The evaluation of psychological needs, i.e. of personal detractors and enhancers within the observations was not part of the study.
Other assessments: In baseline phase, the Mini-Mental-Status Examination was conducted with the PwD. Moreover, sociodemographic data of the residents (e.g. age, gender, degree of care, date of first diagnosis of dementia) were recorded with questionnaires (see Table 4).
Ethical considerations
The study protocol was prepared in accordance with the standards of the Declaration of Helsinki and approved by the Ethics Review Committee and the Data Protection Committee of the Charité. All participants gave their written informed consent to take part in the study. In addition, the study is listed in the German Clinical Trials Register under the number DRKS00011552.
Data Analysis
All quantitative data including those data sets from the DCM observation were collected paper-pencil-based and digitalized using Microsoft Excel. The analysis for the evaluation of DCM observations were carried out using Microsoft Excel as well. The calculation of the percentage time components of the individual profiles of well-being (WIB values) as well as of the behavior categories (BCC values) were carried out. There were two groups per nursing home. A total of six groups were evaluated (for three nursing homes). Observed time units in which no observations were possible or in which conversations between a resident and the mapper took place (coding by BCC "Q") were excluded from the calculations. To enable statistical calculations, the WIB values and BCC values per PwD and observation phase were summed and divided by the total number of observed days of the respective observation phase. Subsequently, the results were analyzed with IBM SPSS Statistics 26 to identify changes in observed behavior and well-being over time. Non-parametric Wilcoxon rank tests were performed for the analysis. To show the changes in well-being and behavior over time, mean values and standard deviation were reported, as the outcomes are based on calculations of percentage time shares.
Instrumentation
The general DCM observation method: The DCM is an observation and evaluation tool which is used to optimize the overall care for PwD. It can be used both as an instrument for developing a person-centered care practice and as a research instrument. Based on an intensive, real-time observation of several hours by one or more observers, the so-called "mappers", the behavior of five to a maximum of eight PwD is recorded simultaneously over a period of four to a maximum of eight hours. The observed behavior is classified and coded into different behavior categories in a time interval of five minutes. The observation takes place exclusively in public spaces and common areas of the care institution (24, 25, 28).
The DCM observation method in the study: Using the DCM method, each resident in the study was observed for five hours in the baseline phase on four days and at the beginning of the intervention phase in week 3 and 4, as well as at the end of the intervention phase in week 7 and 8 on two days. During the last phase (week 13 and 14), the follow-up phase, PwD were mapped again on two days for five hours in the last two weeks.
To ensure an accurate observation, the mapper divided the residents into groups. In two of the three nursing homes, group sizes of five PwD per observation unit (five hours) were selected (a total of two groups with five PwD). In the third care institution, a group size of six PwD per observation unit (five hours) was chosen for the DCM (a total of two groups with 6 PwD). Two PwD had to be excluded due to their death shortly after the start of the study. PwD observations were preferred on days when music interventions took place (e.g. preferred group music therapy and individual music therapy) to understand the effects on well-being and behaviour more effectively.
Up to two different types of information were encoded during observation of the residents: (1) well-being or ill-being (WIB) and (2) Behavior Category Codes (BCC) observed during interactions between caregivers and residents. In terms of well-being and ill-being the mapper gave a WIB value (-5, -3, -1, +1, +3, +5) (see table 2) for each five-minute observation, depending on the signs of well-being shown by the PwD during this five-minute period.
The behavior of the PwD was also coded every five minutes. The DCM tool provides a template for this, covering 23 categories that reflect the range of behaviors that PwD living in institutional settings can display. These categories included behaviors that indicate both an active engagement with the environment (e.g. communication, leisure) and a lack of involvement in that environment (e.g. sleep, non-involvement) (see Table 3). The evaluation of psychological needs, i.e. of personal detractors and enhancers within the observations was not part of the study.
Other assessments: In baseline phase, the Mini-Mental-Status Examination was conducted with the PwD. Moreover, sociodemographic data of the residents (e.g. age, gender, degree of care, date of first diagnosis of dementia) were recorded with questionnaires (see Table 4).
Ethical considerations
The study protocol was prepared in accordance with the standards of the Declaration of Helsinki and approved by the Ethics Review Committee and the Data Protection Committee of the Charité. All participants gave their written informed consent to take part in the study. In addition, the study is listed in the German Clinical Trials Register under the number DRKS00011552.
Data Analysis
All quantitative data including those data sets from the DCM observation were collected paper-pencil-based and digitalized using Microsoft Excel. The analysis for the evaluation of DCM observations were carried out using Microsoft Excel as well. The calculation of the percentage time components of the individual profiles of well-being (WIB values) as well as of the behavior categories (BCC values) were carried out. There were two groups per nursing home. A total of six groups were evaluated (for three nursing homes). Observed time units in which no observations were possible or in which conversations between a resident and the mapper took place (coding by BCC "Q") were excluded from the calculations. To enable statistical calculations, the WIB values and BCC values per PwD and observation phase were summed and divided by the total number of observed days of the respective observation phase. Subsequently, the results were analyzed with IBM SPSS Statistics 26 to identify changes in observed behavior and well-being over time. Non-parametric Wilcoxon rank tests were performed for the analysis. To show the changes in well-being and behavior over time, mean values and standard deviation were reported, as the outcomes are based on calculations of percentage time shares.
Table 1. Overview of the music interventions
| Music intervention | Duration | Frequency | Planned group size | Actual group size (average) | ||
| Temporal rhythm | Total of all sessions | |||||
| Music therapy | Group music therapy | 45 min. | Once a week | 8 times | 5-8 participants | 7.6 participants |
| Individual music therapy | 30 min. | Alternating weeks with group music with movements | 4 times | 1 participant | 8.3 participants | |
| Music-based interventions | Background music during meals | 4 min. | Daily, for every meal (breakfast, lunch, 3pm tea, dinner) | 192 times |
10 participants | No data logging* |
| Group music with movements | 60 min. | Alternating weeks with individual music therapy | 4 times | 10 participants | 6.1 participants | |
| Music program in common room | Approx. 240 min. | Daily | 48 times | 10 participants | No data logging | |
| Individual radio | 30 min. | Twice per day | 96 times | 1 participant | No data logging** | |
* If the music disturbed the PwD during meals, they had the possibility to eat in their room at any time.
** The PwD had the choice of turning off the radio themselves or having it turned off.
Table 2. List of well-and ill-being values (WIB)
| Affect | WIB value | Contact |
| Very happy, joyfully excited, highly positive emotional state | +5 | Very strongly absorbed, drawn deep into the contact, fully involved |
| Satisfied, happy, relaxed, a clearly positive emotional state | +3 | Concentrated, but deflectable, clearly visible contact |
| Neutral emotional state, minor recognizable signs of a positive or negative emotional state | +1 | Attentive, focused on the environment, short or temporary contact |
| Small signs of a negative emotional state | -1 | Withdrawn, without contact |
| Considerable signs of a negative emotional state | -3 | No contact |
| Severe suffering or pressure, very strong signs of a negative emotional state | -5 | No contact |
Results
Study sample
The total sample of PwD (see Table 2) included 30 persons (60.0% female, 60.0% widowed) aged 52 to 97 years (M = 81.4 years) from three different nursing homes. The average MMSE score was 8.5 points (SD = 7.4 points), which corresponds to severe dementia. In addition, the residents preferred to listen to folk music and pop songs (n = 26; 86.7%), followed by classical music and opera (n = 10; 33.3%) as well as pop music/musicals (n = 7; 23.3%) and rock music (n = 3; 10.0%), according to the caregivers.
Well-being
Figure 2 shows the average WIB values of well-being of all participants (WIB scores) over time in total numbers.
Overall, no sufficient change was observed in the course with regard to well-being. On average, the values of well-being remained at +1, which corresponds to a neutral state of affect and focused contact, with no indication of positive or negative sensations.
It was shown that well-being in the intervention phase is significantly lower by 0.22 WIB points (M = 0.99, SD = 0.04) than in the baseline phase (M = 1.01, SD = 0.04) (z = -2.54, p = .01, n = 25). In the course from the intervention phase to the follow-up phase, the value of well-being fell slightly further by 0.01 WIB points. However, no significant difference was found (z = -1.81, p = .07, n = 25).
It can be shown that the use of the music intervention leads to an unchanged state of well-being during the course of the study. This means an effect on the positive or negative change in terms of feelings or involvement of the PwD in the activities of the nursing home (smiles, relaxed facial features, physical and psychological presence, eye contact, communication) cannot be determined.
Study sample
The total sample of PwD (see Table 2) included 30 persons (60.0% female, 60.0% widowed) aged 52 to 97 years (M = 81.4 years) from three different nursing homes. The average MMSE score was 8.5 points (SD = 7.4 points), which corresponds to severe dementia. In addition, the residents preferred to listen to folk music and pop songs (n = 26; 86.7%), followed by classical music and opera (n = 10; 33.3%) as well as pop music/musicals (n = 7; 23.3%) and rock music (n = 3; 10.0%), according to the caregivers.
Well-being
Figure 2 shows the average WIB values of well-being of all participants (WIB scores) over time in total numbers.
Overall, no sufficient change was observed in the course with regard to well-being. On average, the values of well-being remained at +1, which corresponds to a neutral state of affect and focused contact, with no indication of positive or negative sensations.
It was shown that well-being in the intervention phase is significantly lower by 0.22 WIB points (M = 0.99, SD = 0.04) than in the baseline phase (M = 1.01, SD = 0.04) (z = -2.54, p = .01, n = 25). In the course from the intervention phase to the follow-up phase, the value of well-being fell slightly further by 0.01 WIB points. However, no significant difference was found (z = -1.81, p = .07, n = 25).
It can be shown that the use of the music intervention leads to an unchanged state of well-being during the course of the study. This means an effect on the positive or negative change in terms of feelings or involvement of the PwD in the activities of the nursing home (smiles, relaxed facial features, physical and psychological presence, eye contact, communication) cannot be determined.
Table 3. List of behavior category codes (BCC)
| Code | Note | General description of the category |
| A | Articulation | Interact with others verbally or in any other way - without any other recognizable activity |
| B | Borderline (Observation) | Be committed, but in a passive way (observe, look) |
| C | Cool (Cool) | Be uncommitted, withdrawn |
| D | Doing for Self | Self-care |
| E | Expressive | Expressive or creative activities |
| F | Food | Eating or drinking |
| G | Going back | Reminiscence/memory or life review |
| I | Intellectual | Give priority to the use of intellectual capacity |
| J | Joints (Joints and Bones) | Physical or sports activities |
| K | Kum and Go (Come and Go) | Going, standing, or move on their own |
| L | Leisure (Free-time) | Leisure, fun and relaxing&recreative activities |
| N | Nod, land of (Take a nap) | Sleeping or dozing |
| O | Objects | Show a connection to an inanimate object or enter into a relationship with it |
| P | Physical | Receive practical, physical or personal care |
| R | Religion | Be engaged in a religious activity |
| S | Sexual expression | Display a sexual behaviour |
| T | Timalation | Direct involvement of the senses |
| U | Unresponded to | Attempt to communicate without receiving a reaction or response |
| V | Vocational (Work) | Work or work-related activities |
| W | Withstanding | Constant and sustained self-stimulation (no outside reference) |
| X | X-cretion | Occurrences in connection with excretion / excretions |
| Y | Yourself | Interaction in the absence of an observable object or person |
| Z | Zero option | Null option - behavior does not fit into any of the existing categories |
Table 4. Characteristics of the PwD
Note. * Multiple answers possible.
Behavior
Regarding BCC over the course of the study, it was evident that ten of the 23 behavioral categories were observed more frequently in the intervention phase compared to the baseline phase. These BCC were predominantly behaviors associated with physical activation or activity (such as A = Articulation, E = Expressive, J = Joints, K = Kum and go, L = Leisure). Furthermore, it was shown that five of the ten behavioral categories increasingly observed are communication-enhancing behaviors (E = Expressive, G = Going back, J = Joints, L = Leisure, O = Objects). Figure 3 shows the average values of the behavior categories of all participants (BCC scores) over time in %.
There were significant differences during the baseline phase, the intervention phase and the follow-up phase. For example, it was shown that expressive or creative activities (BCC: E) of the participants, such as activities of singing, dancing, making music or using the activities to communicate, were observed significantly stronger (M = 8.41, SD = 8.22) in the intervention phase than in the baseline phase (M = 3.34, SD = 4.78) (z = -3.63, p < 0.001, n = 26). Furthermore, it was observed that physical activities of the participants, such as (instructed) sports exercises, strengthening or physically challenging exercises (BCC: J) in the intervention phase were significantly higher (M = 0.99, SD = 1.82) than at baseline phase (M = 0.00, SD = 0.00) (z = -2.37, p = .02, n = 26). It was also shown that work-related activities (BCC: V) of the participants, such as washing dishes or similar, were observed significantly less in the intervention phase (M = 2.01, SD = 6.99) compared to the baseline phase (M = 4.77, SD = 9.26) (z = -2.76, p = .01, n = 26).
| Characteristics | Forms | PwD (n=30) | |
| sex | Female Male |
18 12 |
|
| Age [Ø years, ± SD] | Total Female Male |
81.4 ± 9.0 82.7 ± 8.1 79.5 ± 10.3 |
|
| MMSE [Ø points, ± SD] | Total | 8.5 ± 7.4 | |
| Favorite music genre (in %)* | Folk music Classic Songs/Opera Pop music Rock music Jazz/Blues |
86.7 33.3 23.3 10.0 0.0 |
|
Behavior
Regarding BCC over the course of the study, it was evident that ten of the 23 behavioral categories were observed more frequently in the intervention phase compared to the baseline phase. These BCC were predominantly behaviors associated with physical activation or activity (such as A = Articulation, E = Expressive, J = Joints, K = Kum and go, L = Leisure). Furthermore, it was shown that five of the ten behavioral categories increasingly observed are communication-enhancing behaviors (E = Expressive, G = Going back, J = Joints, L = Leisure, O = Objects). Figure 3 shows the average values of the behavior categories of all participants (BCC scores) over time in %.
There were significant differences during the baseline phase, the intervention phase and the follow-up phase. For example, it was shown that expressive or creative activities (BCC: E) of the participants, such as activities of singing, dancing, making music or using the activities to communicate, were observed significantly stronger (M = 8.41, SD = 8.22) in the intervention phase than in the baseline phase (M = 3.34, SD = 4.78) (z = -3.63, p < 0.001, n = 26). Furthermore, it was observed that physical activities of the participants, such as (instructed) sports exercises, strengthening or physically challenging exercises (BCC: J) in the intervention phase were significantly higher (M = 0.99, SD = 1.82) than at baseline phase (M = 0.00, SD = 0.00) (z = -2.37, p = .02, n = 26). It was also shown that work-related activities (BCC: V) of the participants, such as washing dishes or similar, were observed significantly less in the intervention phase (M = 2.01, SD = 6.99) compared to the baseline phase (M = 4.77, SD = 9.26) (z = -2.76, p = .01, n = 26).
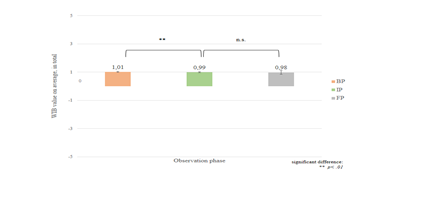
Figure 2. WIB value on average, in total
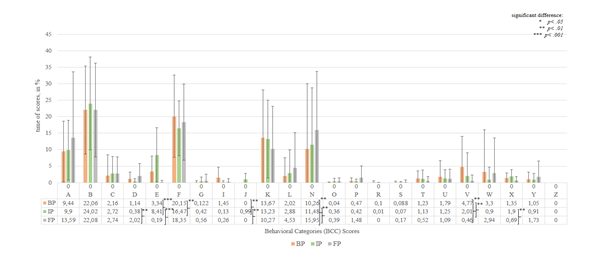
Figure 3. BCC time scores in %
There were significant differences during the baseline phase, the intervention phase and the follow-up phase. For example, it was shown that expressive or creative activities (BCC: E) of the participants, such as activities of singing, dancing, making music or using the activities to communicate, were observed significantly stronger (M = 8.41, SD = 8.22) in the intervention phase than in the baseline phase (M = 3.34, SD = 4.78) (z = -3.63, p < .001, n = 26). Furthermore, it was observed that physical activities of the participants, such as (instructed) sports exercises, strengthening or physically challenging exercises (BCC: J) in the intervention phase were significantly higher (M = 0.99, SD = 1.82) than at baseline phase (M = 0.00, SD = 0.00) (z = -2.37, p = .02, n = 26). It was also shown that work-related activities (BCC: V) of the participants, such as washing dishes or similar, were observed significantly less in the intervention phase (M= 2.01, SD = 6.99) compared to the baseline phase (M = 4.77, SD = 9.26) (z = -2.76, p = .01, n = 26).
Discussion
This study showed the positive effect of music therapy and music-based interventions on specific behaviors of PwD in nursing homes, which were observed over 14 weeks using the DCM method. Moreover, the well-being during the observation remained almost constant over the course of the study.
Behaviors associated with increased physical activity were observed significantly more than other behaviors attributable to apathetic behavior and apathy (BCC: C). This could be due to the fact that there were more programs of receptive music therapy/music-based interventions (e.g. group music with movements, individual radio, background music), which had an influence on the physical activity of PwD, than programs of (inter)active music therapy (13,15). Tsoi and colleagues showed in a systematic review and meta-analysis 2018, in which they compared the effects of receptive and interactive music therapy on the cognitive functions and behavioral symptoms of PwD, a reduction in behavioral symptoms in participants of receptive music therapy (15). Shimizu and other researchers also found out in a RCT with MCI patients and movement music therapy that the use of music can improve flexibility, functional mobility, gait, and muscle endurance (13).
It was also found that there was an increase in behaviors associated with communication-enhancing activities, resulting in the enhancement of cognitive function, improvement in BPSD (14) and emotional expression (16,17). For example, the study by Gómez Gallego also showed significant improvements in memory, orientation, depression, anxiety and language disorders (14). Furthermore, Huber and colleagues in the Music and Memory Study of 2020 showed that positive emotions were shown significantly more often than negative emotions during music listening (17). Unlike the results from other studies, no significant differences were observed with regard to decrease in apathic behavior (29) and improvement in quality of life (19). One cause may be the death of residents during the period of the study. Thus, the changes in well-being and behavior were observed continuously and an evaluation and calculation of statistical significance was not performed. It should also be noted that not all PwDs feel equally affected by musical interventions. For example, some participants in this study may not have experienced any proven stimulation of their cognitive functions (30) and thus may not have experienced any effects in BPSD. In addition, no effect in well-being was manifested. However, in order to provide a holistic perspective of the impact of music therapy and music-based interventions, it would have been necessary to observe and analyze all the needs of person-centered care - specifically the quality of life (31, 26).
With regard to the evaluation of potential care processes in long-term care facilities using DCM, the high demands on time, financial and human resources and efforts should be taken into account in future (long-term) studies (32, 33). Alternative methods of evaluating or validating data offer more cost-effective, less complex qualitative or quantitative (online) surveys using questionnaires or interviews.
Furthermore, the validity of the DCM method modified in this study must be considered. As other authors have reported in studies, the comparability of results from other studies or the comparability with valid, quantitative assessments (e.g. Quality of Life) is limited (34, 35, 32). The same concerns about reliability and internal consistency exist, which queried the use of the DCM tool as a research tool (36).
Conclusion
Overall, the results of the study demonstrate the positive effects of music therapy and music-based interventions on certain behaviors observed using the DCM method. Nevertheless, valid assessments and a comparison of interval and control groups (RCT) should be used in future studies. Furthermore, DCM in its original approach should be used and maintained as an observation method to improve processes of person-centered care.
Study limitations
As the study focused on observing as many PwD as possible, it was not feasible, for example, to observe residents who were mostly in their rooms. Therefore, some of the study data were missing. Furthermore, improvements in the outcome quality of life could not be identified, as personal enhancers and detractions of caregivers were not observed. Moreover, no interrater reliability could be calculated, since observations of two mappers were partly carried out simultaneously and personnel resources were reduced.
Funding
This research received specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
We know of none declared conflicts of interest associated with this publication.
Acknowledgements
This work was supported by the German Federal Ministry of Education and Research (BMBF) under grant number 16SV7371. Responsibility for the contents of this publication lies with the authors. The aim of the wider project was to develop a musical system for people with dementia. This was a joint project that ended in September 2018.
Authors' contributions
RD conceived, designed, wrote the article, performed the study and evaluated the data. CE performed the study, revised and edited the manuscript. DF evaluated the data and reviewed the study contents. All authors read and approved the final manuscript.
References
Discussion
This study showed the positive effect of music therapy and music-based interventions on specific behaviors of PwD in nursing homes, which were observed over 14 weeks using the DCM method. Moreover, the well-being during the observation remained almost constant over the course of the study.
Behaviors associated with increased physical activity were observed significantly more than other behaviors attributable to apathetic behavior and apathy (BCC: C). This could be due to the fact that there were more programs of receptive music therapy/music-based interventions (e.g. group music with movements, individual radio, background music), which had an influence on the physical activity of PwD, than programs of (inter)active music therapy (13,15). Tsoi and colleagues showed in a systematic review and meta-analysis 2018, in which they compared the effects of receptive and interactive music therapy on the cognitive functions and behavioral symptoms of PwD, a reduction in behavioral symptoms in participants of receptive music therapy (15). Shimizu and other researchers also found out in a RCT with MCI patients and movement music therapy that the use of music can improve flexibility, functional mobility, gait, and muscle endurance (13).
It was also found that there was an increase in behaviors associated with communication-enhancing activities, resulting in the enhancement of cognitive function, improvement in BPSD (14) and emotional expression (16,17). For example, the study by Gómez Gallego also showed significant improvements in memory, orientation, depression, anxiety and language disorders (14). Furthermore, Huber and colleagues in the Music and Memory Study of 2020 showed that positive emotions were shown significantly more often than negative emotions during music listening (17). Unlike the results from other studies, no significant differences were observed with regard to decrease in apathic behavior (29) and improvement in quality of life (19). One cause may be the death of residents during the period of the study. Thus, the changes in well-being and behavior were observed continuously and an evaluation and calculation of statistical significance was not performed. It should also be noted that not all PwDs feel equally affected by musical interventions. For example, some participants in this study may not have experienced any proven stimulation of their cognitive functions (30) and thus may not have experienced any effects in BPSD. In addition, no effect in well-being was manifested. However, in order to provide a holistic perspective of the impact of music therapy and music-based interventions, it would have been necessary to observe and analyze all the needs of person-centered care - specifically the quality of life (31, 26).
With regard to the evaluation of potential care processes in long-term care facilities using DCM, the high demands on time, financial and human resources and efforts should be taken into account in future (long-term) studies (32, 33). Alternative methods of evaluating or validating data offer more cost-effective, less complex qualitative or quantitative (online) surveys using questionnaires or interviews.
Furthermore, the validity of the DCM method modified in this study must be considered. As other authors have reported in studies, the comparability of results from other studies or the comparability with valid, quantitative assessments (e.g. Quality of Life) is limited (34, 35, 32). The same concerns about reliability and internal consistency exist, which queried the use of the DCM tool as a research tool (36).
Conclusion
Overall, the results of the study demonstrate the positive effects of music therapy and music-based interventions on certain behaviors observed using the DCM method. Nevertheless, valid assessments and a comparison of interval and control groups (RCT) should be used in future studies. Furthermore, DCM in its original approach should be used and maintained as an observation method to improve processes of person-centered care.
Study limitations
As the study focused on observing as many PwD as possible, it was not feasible, for example, to observe residents who were mostly in their rooms. Therefore, some of the study data were missing. Furthermore, improvements in the outcome quality of life could not be identified, as personal enhancers and detractions of caregivers were not observed. Moreover, no interrater reliability could be calculated, since observations of two mappers were partly carried out simultaneously and personnel resources were reduced.
Funding
This research received specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
We know of none declared conflicts of interest associated with this publication.
Acknowledgements
This work was supported by the German Federal Ministry of Education and Research (BMBF) under grant number 16SV7371. Responsibility for the contents of this publication lies with the authors. The aim of the wider project was to develop a musical system for people with dementia. This was a joint project that ended in September 2018.
Authors' contributions
RD conceived, designed, wrote the article, performed the study and evaluated the data. CE performed the study, revised and edited the manuscript. DF evaluated the data and reviewed the study contents. All authors read and approved the final manuscript.
References
- World Health Organization (WHO). Dementia [Internet]. 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/dementia
- Alzheimer’s Association. What Is Dementia? [Internet]. Alzheimer’s Disease and Dementia. 2020 [cited 2020 May 22]. Available from: https://alz.org/alzheimers-dementia/what-is-dementia
- Dilling Ht, Mombour W, Schmidt MH, World Health Organization. Internationale Klassifikation psychischer Störungen: ICD-10, Kapitel V (F)- klinisch-diagnostische Leitlinien [Internet]. 1991 [cited 2020 May 20]. Available from: https://apps.who.int/iris/handle/10665/38221
- OECD. Addressing dementia - the OECD response [Internet]. OECD iLibrary: 2015 [cited 2020 May 22]. Available from: https://read.oecd-ilibrary.org/social-issues-migration-health/addressing-dementia_9789264231726-en
- Alzheimer's Disease International, Wimo A, Ali GC, Guerchet M, Prince M, Prina M, et al. World Alzheimer Report 2015: The Global Impact of Dementia [Internet]. 2015. Available from: https://www.alz.co.uk/research/world-report-2015/
- Alzheimer Disease International. Improving dementia care worldwide: ideas and advice on developing and implementing a national dementia plan [Internet]. London; 2013. P 60. Available from: https://www.alz.co.uk/sites/default/files/pdfs/global-dementia-plan-report-ENGLISH.pdf
- Testad I, Aasland AM, Aarsland D. Prevalence and correlates of disruptive behavior in patients in Norwegian nursing homes. International Journal of Geriatric Psychiatry. 2007; 22(9): 916–21.
- Sury L, Burns K, Brodaty H. Moving in: adjustment of people living with dementia going into a nursing home and their families. International Psychogeriatrics. 2013; 25(6): 867–76.
- Auer SR, Höfler M, Linsmayer E, Beránková A, Prieschl D, Ratajczak P, et al. Cross-sectional study of prevalence of dementia, behavioural symptoms, mobility, pain and other health parameters in nursing homes in Austria and the Czech Republic: results from the DEMDATA project. BMC Geriatrics. 2018; 18(178): 1-13.
- Jørgensen LB, Thorleifsson BM, Selbæk G, Šaltytė Benth J, Helvik A-S. Physical diagnoses in nursing home residents - is dementia or severity of dementia of importance?. BMC Geriatrics. 2018; 18: 1-14.
- Ahmed M, Malik M, Teselink J, Lanctôt KL, Herrmann N. Current agents in development for treating behavioral and psychological symptoms associated with dementia. Drugs & Aging. 2019; 36(7): 589–605.
- Gómez-Romero M, Jiménez-Palomares M, Rodríguez-Mansilla J, Flores-Nieto A, Garrido-Ardila EM, González-López-Arza MV. Benefits of music therapy on behaviour disorders in subjects diagnosed with dementia: A systematic review. Neurología (English Edition). 2017; 32(4): 253–63.
- Shimizu N, Umemura T, Matsunaga M, Hirai T. Effects of movement music therapy with a percussion instrument on physical and frontal lobe function in older adults with mild cognitive impairment: a randomized controlled trial. Aging & Mental Health. 2018; 22(12): 1614–26.
- Gómez Gallego M, Gómez García J. Music therapy and Alzheimer’s disease: Cognitive, psychological, and behavioural effects. Neurología (English Edition). 2017; 32(5): 300–8.
- Tsoi KKF, Chan JYC, Ng Y-M, Lee MMY, Kwok TCY, Wong SYS. Receptive music therapy is more effective than interactive music therapy to relieve behavioral and psychological symptoms of dementia: a systematic review and meta-analysis. Journal of the American Medical Directors Association. 2018; 19(7): 568-576.
- Elliott M, Gardner P. The role of music in the lives of older adults with dementia ageing in place: A scoping review. Dementia. 2018; 17(2): 199–213.
- Huber A, Oppikofer S, Meister L, Langensteiner F, Meier N, Seifert A. Music & memory: the impact of individualized music listening on depression, agitation, and positive emotions in persons with dementia. Activities, Adaptation & Aging. 2020; 1–15.
- 18.Liesk J, Hartogh T, Kalbe E. Kognitive stimulation und musikintervention bei stationär versorgten menschen mit demenz: eine pilotstudie, probleme und perspektiven. Zeitschrift für Gerontologie + Geriatrie. 2015; 48(3): 275–81.
- Cho HK. The effects of music therapy-singing group on quality of life and affect of persons with dementia: a randomized controlled trial. Frontiers in Medicine. 2018; 5: 1-13.
- Thomas KS, Baier R, Kosar C, Ogarek J, Trepman A, Mor V. Individualized music program is associated with improved outcomes for U.S. nursing home residents with dementia. The American Journal of Geriatric Psychiatry. 2017; 25(9): 931–8.
- Hebert CA, Hancock K, McConnell ES. Implementation of individualized music in long-term care: application of the PARiHS framework. Journal of Gerontological Nursing. 2018; 44(8): 29–38.
- Weise L, Jakob E, Töpfer NF, Wilz G. Study protocol: individualized music for people with dementia - improvement of quality of life and social participation for people with dementia in institutional care. BMC Geriatrics. 2018; 18(313): 1-8.
- Weise L, Töpfer NF, Deux J, Wilz G. Feasibility and effects of individualized recorded music for people with dementia: A pilot RCT study. Nordic Journal of Music Therapy. 2020; 29(1): 39–56.
- Kitwood T. The dialectics of dementia: with particular reference to Alzheimer’s disease. Ageing & Society. 1990; 10(2): 177–96.
- Kitwood T, Bredin K. Towards a theory of dementia care: personhood and well-being. Ageing & Society. 1992; 12(3): 269–87.
- Dichter MN, Quasdorf T, Schwab CGG, Trutschel D, Haastert B, Riesner C, et al. Dementia care mapping: effects on residents’ quality of life and challenging behavior in German nursing homes. A quasi-experimental trial. International Psychogeriatrics. 2015; 27(11): 1875–92.
- Surr CA, Griffiths AW, Kelley R. Implementing Dementia Care Mapping as a practice development tool in dementia care services: a systematic review [Internet]. Clinical Interventions in Aging. 2018 [cited 2019 Oct 4]. Available from: https://www.dovepress.com/implementing-dementia-care-mapping-as-a-practice-development-tool-in-d-peer-reviewed-article-CIA
- Kitwood T. Person and process in dementia. International Journal of Geriatric Psychiatry. 1993; 8(7): 541–5.
- Tang Q, Zhou Y, Yang S, Wong TKS, Smith GD, Yang Z, et al. Effect of music intervention on apathy in nursing home residents with dementia. Geriatric Nursing. 2018; 39(4): 471–6.
- Han JW, Lee H, Hong JW, Kim K, Kim T, Byun HJ, et al. Multimodal cognitive enhancement therapy for patients with mild cognitive impairment and mild dementia: a multi- center, randomized, controlled, double-blind, crossover trial. Journal of Alzheimer's Disease. 2017; 55(2): 787–96.
- Innes A, Surr C. Measuring the well-being of people with dementia living in formal care settings: The use of dementia care mapping. Aging & Mental Health. 2001; 5(3): 258–68.
- Sloane PD, Brooker D, Cohen L, Douglass C, Edelman P, Fulton BR, et al. Dementia care mapping as a research tool. International Journal of Geriatric Psychiatry. 2007; 22(6): 580–9.
- Surr CA, Walwyn REA, Lilley-Kelly A, Cicero R, Meads D, Ballard C, et al. Evaluating the effectiveness and cost-effectiveness of Dementia Care mapping TM to enable person-centred care for people with dementia and their carers (DCM-EPIC) in care homes: study protocol for a randomised controlled trial. Trials. 2016; 17(1): 1-17.
- Beavis D, Simpson S, Graham I. A literature review of dementia care mapping: methodological considerations and efficacy. Journal of Psychiatric and Mental Health Nursing. 2002; 9(6): 725–36.
- Chenoweth L, Jeon Y-H. Determining the efficacy of dementia care mapping as an outcome measure and a process for change: A pilot study. Aging & Mental Health. 2007; 11(3): 237–45.
- Villar F, Vila-Miravent J, Celdrán M, Fernández E. Assessing the well-being of patients with dementia: validity and reliability of the Spanish version of the Dementia Care Mapping (DCM) tool / La evaluación del bienestar en pacientes con demencia: validez y fiabilidad de la versión española del Dementia Care Mapping (DCM). Estudios de Psicología. 2015; 36(2): 389–412.
Type of Study: Research |
Subject:
General
Received: 2020/07/16 | Accepted: 2020/10/5 | Published: 2020/12/28
Received: 2020/07/16 | Accepted: 2020/10/5 | Published: 2020/12/28
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |