BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ehj.ssu.ac.ir/article-1-177-en.html
The Effectiveness of a Chronic Disease Self-Management Program for Elderly People: a Systematic Review
Khairunnisa Mansoor *1, Hussain Maqbool Ahmed Khuwaja 1
1. School of Nursing and Midwifery, Aga Khan University, Karachi, Pakistan
Received 10 Oct 2019
Accepted 21 Jun 2020
A B S T R A C T
Introduction: Elderly population is increasing in Pakistan. Majority of people aged 50 – 64, suffer from two or more chronic conditions. Care of elderly people is sub-optimal. Healthcare system has limited resources to provide healthcare support to elderly people. Thus, there is need to empower the elderly to self-manage their health conditions. Chronic Disease Self-Management Program (CDSMP) is the most widely accepted self-management patient education program. It is designed to help people to gain confidence and skills to better manage their chronic conditions. Evidence of the effectiveness of CDSMP specifically for elderly people aged 60 years and above is lacking. Therefore, the aim of this systematic review was to determine the effects of the program among chronically ill elderly people.
Methods: MEDLINED, CINHAL, EMBASE, PSYINFO, JBI and ASSIA were searched between April and May, 2020 for studies that tested the effects of generic CDSMP. A total of 750 articles were identified, of which 5 were included in the core review (four randomized controlled trials and one quasi-experimental).
Results: Eligible 5 studies yielded 2971 participants (mean aged 60.4 to 76.0 years). Elder people who participated in CDSMP improved their self-efficacy to manage disease in general and to manage symptoms. The effects on health status were mixed. Self-rated health and health distress showed significant improvement. Some health behaviours showed improvement, particularly exercise component showed significant improvement. For health services utilization, there was no improvement.
Conclusion: The result of this review suggests that CDSMP is beneficial for elderly people who attended the structured CDSMP either through a trained care provider or layman. Experimental studies in low and middle income countries, with large sample sizes are suggested to further understand the impact of CDSMP.
Keywords: CDSMP, Aged, Health Status, Self-Efficacy, Health Behaviours
Introduction
The global numbers of ageing population aged 60 years or above have tripled between 1950 and 2000. It is projected that during the next four to five decades, two billion elderly persons will be alive, which means the world’s elderly population will be tripled by 2050 (1). Out of the population of people aged 60 years and above, two-thirds, live in the developing world (1). Pakistan as a developing country has a total population of 207,774,520 (2). The proportion of older people in Pakistan is becoming challenging. According to the local data, in Pakistan the proportion of population 60 years and above was 6.5% in 2012 and projected to increase to almost 16% of the total population by 2050. When the older population increases at such a rapid rate, the challenges in making the imperative changes to health care are undoubtedly great. While developed countries may be able to accommodate gradual population ageing, for many developing countries it is difficult to respond to rapid ageing with very limited economic resources (3). This is indicating for urgent need of innovative policy responses.
Alongside the speed at which developing countries are projected to age and the limited economic resources for responding to this transition, the burden of disease is also shifting both from the young to the old and from communicable (infectious diseases) to non-communicable (chronic) diseases (3-5). Globally, each year 71% of all death occurs due to chronic diseases (6). In Pakistan, non-communicable diseases projected to account 58% of all death that reflects death due to chronic diseases are more than morbidity due to communicable diseases (7).
Changes in family structure in under developed countries add to the challenge of ensuring adequate health care for this population. In the past, Pakistan had an extended family system. As a result, most elderly people received support from their family. However, recently family size is shrinking due to the migration of young adult children to other countries in search of employment and career advancement (8). This often results in parents who were once close to their children living alone, who slowly age and experience decline in quality of life (9).
It seems clear that demographic transition (an ageing society and the emergence of nuclear families) combined with epidemiological transition (decline in infections and rise in chronic disorders) are becoming a problem for health care systems with increasing demand but limited human and financial resources. The care for older adults with chronic disease is yet suboptimal in Pakistan. Elderly care is not recognized as a separate specialty. Furthermore, the health care system is based on a weak infra-structure and there is lack of residential and rehabilitation facilities resulting in the neglect of the health care needs of the elderly population (10).
As elderly people often suffer from more than one chronic disease, the Chronic Disease Self-Management Program (CDSMP) approach is highly applicable for this group of population. The CDSMP for patient education aims at better management of chronic conditions and helping the patients to take control of their life using a self-management approach (11, 12). This systematic review is the first to assess the effectiveness of generic CDSMP specifically among the elderly population. This paper aims to identify whether this program is explicitly beneficial and applicable for people aged 60 years and above. This review aimed to evaluate the impact of CDSMP program against usual care or the wait-list group among older adults with mean age of 60 and above, in relation to four outcomes; health status, self-efficacy, health behaviour and health service utilization. The outcomes were evaluated after six months of intervention delivered over a period of six weeks. It is anticipated that this systematic review will generate new knowledge and produce reliable and valid evidence for health care policy makers in Pakistan.
Methods
Search strategy
A three-step search strategy was utilized in this review. An initial limited search of MEDLINE and CINAHL were performed followed by analysis of the text words contained in the title and abstract, and of the index terms used to describe an article. A second search using all identified keywords and index terms were then undertaken across all included databases [Cumulative Index to Nursing and Allied Health Literature (CINAHL), MEDLINE, Excerpta Medica Database (EMBASE), Cochrane Library, PsycINFO, ASSIA, JBI COnNECT (Clinical Online Network of Evidence for Care and Therapeutics)] to reduce the possibility of missing relevant literature. Thirdly, a hand search of other sources of studies such as reference lists and bibliographies of all retrieved articles was screened to identify any additional relevant studies (13). Maximizing the amount of data available from all relevant studies minimizes the chance effects and publication bias (14, 15). Table 1 includes the search terms used for this study.
The literature search was conducted between April and May, 2020. Additionally, the review was not limited to any time interval. Studies published in the English language were considered. This review was planned to include elderly people aged 60 years or above. However, few studies were found that have investigated specifically this age group. Therefore, the inclusion criteria were amended to consider the participant mean age of 60 years or above. A decision was made to include those studies that have documented participant mean age 60 years or above rather 60 years or above to avoid inclusion bias for excluding relevant studies (16) and to reduce the possibility of reviewer selection on the basis of studies result (17).
Thus, review included elderly people mean aged 60 years or above, of either sex, belonging to any ethnicity, had one or more chronic conditions and lived in community; and excluded participants with mental health diseases and cancer disease who had received chemotherapy or radiation within past year. Furthermore, we included CDSMP that were precise and delivered in a workshop format. These sessions were conducted for two and a half hours, once a week, for six weeks and facilitated by two trained leaders, one or both of whom were non-health professionals with chronic diseases themselves. Studies were included that had direct interaction between the participants and the tutor such as face-to-face workshop format for a group. This review took an account of those trials that offered formal CDSMP in the form of workshop with distribution of materials such as self-help workbooks, provision of written materials or literature, tapes, or DVDs (Digital Video Discs) to the intervention group. Studies were considered for inclusion in the review if they followed seven themes of CDSMP content (including cognitive symptom management, exercise, communication, dealing with anger and depression, problem solving, contracting service providers, and advanced directives (18). Studies included comparators such as usual care or wait-list group. Usual care means no education session or only written or verbal health information. Wait-list groups are those who got usual care for six months and received the CDSMP course six months after the treatment group. The primary outcomes of interest included self-efficacy, health status and health behaviour; secondary outcome included health service utilization. Studies were included that had six months follow up.
Data collection and analysis
Study selection
Following the PRISMA guidelines, when the title and abstract were inconclusive, the full text was retrieved for further assessment (19). Overall, 732 studies were identified from different data base searches. The titles and abstracts of these studies were screened for duplication and relevancy to the review. This led to exclusion of 703 clearly duplicated or irrelevant studies. Full articles and abstracts of the remaining 29 studies were retrieved and scrutinized against inclusion and exclusion criteria. This
resulted in further exclusion of 24 more studies. Finally, 5 studies, 4 RCTs and 1 quasi-experimental study were included in the review. The PRISMA flow chart of search method is showed in figure 1.
Data extraction, management and review
The JBI-MAStARI critical appraisal tool (20) was used to identify studies of sufficient quality to include. Methodological quality scores of included studies ranged from 5 to 10. Details of quality appraisal are reported in tables 2 and 3. Quality assessment was first performed by primary author and independently performed by second author. Both authors extracted data in the form of table identifying study author, study country, study sample size, participant characteristics (such as age and gender), study designs, description of interventions (number of sessions, and delivered by), and outcomes.
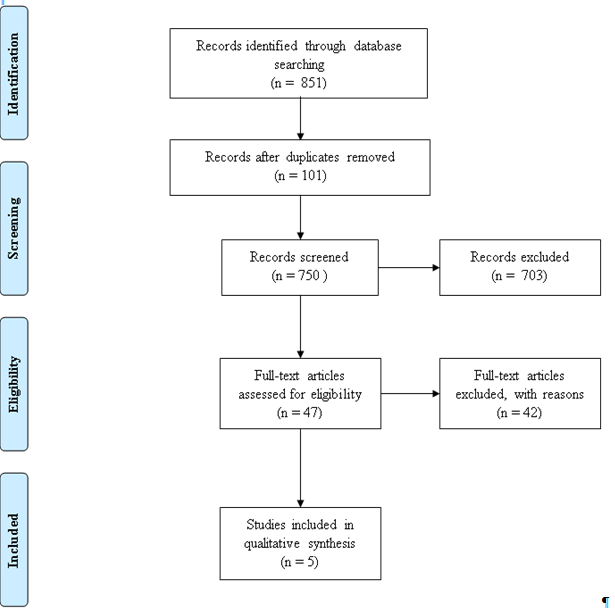
Figure 1: PRISMA flow diagram for study selection
Table 1. Search strategy
|
Population |
Intervention |
Comparison |
Outcomes |
|
“Elderly” OR “Older Adults” OR “Geriatric” |
“Self-Management” OR “Self Management” OR “Self Management” AND “Chronic Disease” OR “CDSMP” |
“Wait-Listed” OR “Usual Care” |
“Self-Efficacy” OR “Health Status” OR “Health Behaviour” OR “Healthcare Utilization” |
Note: Boolean Operator “AND” was used to make combinations
Table 2. Quality score of RCTs based on JBI critical appraisal tool for RCTs
|
Author (Year) Population |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
Score |
Quality |
|
Lorig et al. (1999) USA |
Y |
N |
N |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
8 |
High |
|
Fu Dongbo et al. (2003) Urban communities in Shanghai, China |
Y |
N |
N |
Y |
N |
Y |
Y |
Y |
Y |
Y |
7 |
Moderate |
|
Swerissen et al. (2006) Vietnamese, Chinese, Italian and Greek backgrounds living in Victoria, Australia |
Y |
N |
N |
N |
U |
Y |
Y |
Y |
Y |
N |
5 |
Moderate |
|
Elzen et al. (2007) Netherlands (Dutch) |
Y |
N |
N |
Y |
U |
Y |
Y |
Y |
Y |
Y |
7 |
Moderate |
Note: Rating score is from 1 (lowest) to 10 (highest); Y= Yes; N=No; U= Unclear.
Quality score were categorized into three groups: Low: 1-4, Moderate: 5-7, and High: 8-10
Table 3. Quality score of quasi-experimental studies based on JBI critical appraisal tool for cohort studies (modified)
|
Author (Year) Population |
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
Total |
Quality |
|
Chan et al. (2011) Hong Kong |
Y |
N |
N |
Y |
Y |
Y |
Y |
Y |
Y |
7 |
Moderate |
Note: Rating score is from 1 (lowest) to 10 (highest); Y= Yes; N=No; U= Unclear.
Quality score were categorized into three groups: Low: 1-4, Moderate: 5-7, and High: 8
Results
Four trials (21-24) and one quasi-experimental study (25) met all the review criteria. A list of excluded studies and the reason for their exclusion is provided in Supplementary Data. All the included studies were based in a community setting and conducted in different parts of the world such as USA, China, Australia, Netherlands and Hong Kong.
In total, 2971 participants were included in the studies reviewed. Participants were recruited via advertisements in the mass media, posters at community centres, referrals from flyers left in community clinics and interpersonal persuasion. Full demographic details of the participants in the intervention and control groups are provided in table 4. The mean ages of the participants were 60.4 to 76.0 in all included studies reflecting that most of the participants belong to old age group. Although five studies focused on both gender, females’ numbers were significantly high in each study. This reflects the data that women have higher life expectancies than men. The mean number of years of education was 8.9. USA older people were highly educated (mean education years = 15) as compared to Hong Kong (mean education years = 4) compared to other studies as shown in table 4. This suggests that in most of the program elderly participants were educated at least up to primary level.
Except Elzen et al. all four studies reported the mean number of disease ranges from 2.09 to 2.28 in intervention group and 1.95 to 2.39 in control group (refer Supplementary Data). However, none of the studies identified the severity and duration of disease. In addition, most of participants having arthritis as compared to the other chronic conditions. This reciprocates the fact that arthritis is common in older people. The chronic disease diagnosis was confirmed by a physician in a study conducted in USA and was self-reported in other four studies.
Although, the overall withdrawal rate of participant from the program slightly high in only one study (23), participant’s weekly attendance rate in each program was satisfactory with the majority of participants attending all six sessions and completing the program (refer Supplementary Data). The overall mean program attendance rate ranged between 3 - 5.6 in four studies and one study (22) had not reported this rate. It seems that many of the programs were successful as attendance rate of participants was satisfactory. The studies included in the review evaluated a broadly similar intervention of generic chronic disease self-management program. Studies followed a formal syllabus for the Chronic Disease Self-Management Program (CDSMP) developed by Lorig at Standford University Patient Education Research Centre. However, studies had modified and translated the original version for Chinese people in Shanghai and Hong Kong (22, 25), Vietnamese, Chinese, Greek and Italian people in Victoria (23) and for Dutch people in Netherland (24).
The program format was consistent between studies. Courses were conducted over six or seven weeks in two and a half hour each at community based facilities such as churches, senior citizens and community centres. Each study has taught the program in group of 10 - 15 participants by two trained leaders. Although, it is reported that in all studies leaders were trained to teach the program, there was unclear information about how they recruited leaders. Furthermore, studies did not explain the educational background and experience of the lay leader. However, the leaders taught the program following a standardised leader’s manual. CDSMP was developed by Lorig and she also developed the validated and reliable tool to evaluate the patient education and health promotion program (26). It is observed that Lorig and colleagues have used this tool to evaluate the CDSMP in USA and then all subsequent studies used the same outcomes to evaluate the program in different population. Although, three studies (22, 23, 25) had used the same tool to measure the outcome, they had made changes in the tool according to the culture. A study of Elzen et al. used different tool to evaluate the CDSMP outcome of self-efficacy and health status and did not examine the outcome of health service utilization. However, to evaluate the outcome of self-management behaviour they adopted the original tool. There were 20 different sub-outcomes under the four broad outcomes that include self-efficacy, health status, and health behaviour and health service utilization. It was examined that not all four studies considered 20 outcomes consistently. Some of the studies have considered 17 or 18 sub-outcomes under the four broad outcomes. The significance of these outcomes is presented in table 5 and narrative description has been presented below.
Three RCTs and one quasi-experimental study examined the self-efficacy and measured the two components of the self-efficacy. These components were self-efficacy to manage disease in general and self-efficacy to manage the symptoms. In Fu et al. study, the treatment group had significant improvements in both measures of self-efficacy (both p = 0.001). A second RCT by Swerissen et al. found a statistically significant improvement in self-efficacy (p < 0.000). The third RCT by Elzen et al. reported no difference in self-efficacy between the intervention and the control group. However, this study sample size was small. Further, they used Dutched version of the General Self-Efficacy Scale (27) to measure this outcome. This scale consists of 16 questions, scored on a 5-point Liker scale of the dimension agree/disagree, a higher score indicating a higher level of self-efficacy.
Lastly, a quasi-experimental study by Chan et al. using a control group with pre-test design found difference in managing self-efficacy for symptoms and managing disease in general. The intervention group demonstrated significant improvements (both p < 0.0005) while control group showed deterioration in both self-efficacies.
This seems most likely that older people who participated in CDSMP can improved their self-efficacy significantly to manage disease in general and to manage symptoms compare to those who had not participated the CDSMP.
Four studies used the seven to nine components to measure the health status of the participants. These components were self-rated health, energy/fatigue, health distress, shortness of breath, pain, disability, psychological wellbeing/depression, social/role activity limitation, and illness intrusiveness. Each component is self-rated by the participants. In all included studies (21-23, 25) intervention participants demonstrated significantly better outcomes for measures of self-rated health (p < 0.02) and health distress (p < 0.04) than control subjects. However, the result was varied for other symptoms measuring the health status. Lorig et al. found no significant differences for pain and physical discomfort, shortness of breath, or psychological well-being between base line and the 6 months’ follow-ups. On the other hand, Fu et al. reported that treatment group also had significant improvement in pain, shortness of breath, and psychological wellbeing or depression. Swerissen et al. mentioned that there were no significance differences between the groups who attended the CDSMP and who did not attend the CDSMP on the shortness of breath (p = 0.67), disability (p = .426), depression (p = 0.422), social role/activity limitation (p = 0.067) and illness intrusiveness (p = 0.076).
Elzen et al. used RAND-36 to measure the health status. This study reported only two components such as physical component and mental component to demonstrate the health status of the intervention and control group. Elzen et al. showed no improvement in physical and mental health status of 68 subjects that were involved in intervention and control group at immediately after the course had finished (T1), and six months after the end of the course (T2) (Physical component T1, p = 0.29 and T2, p = 0.45 Mental component T1, p = 0.35 and T2 p = 0.46). It could be the reason that they used different scale to measure the outcome. This seems that there is an inconsistency in the improvement of different symptoms of health status of the older people. However, overall older people who participated in the CDSMP showed some areas of improvement in their health status.
All five studies evaluated health behaviours. There were four sub components of the self-management behaviour. These components included aerobic exercise, stretching and strengthening exercise, cognitive symptom management and communication with general physician. However, Swerissen et al. evaluated only two components including: exercise and cognitive symptom management. Elzen et al. also measured only two components including: exercise and communication with physician.
Lorig et al. identified significant improvement in all the four items of the self-management behaviour. Fu et al. showed improvement in cognitive symptom management and aerobic exercise but not in stretching and strengthening exercise and communication with physician. Swerissen et al. showed improvement in cognitive symptom management and exercise. These results were similar to Lorig et al. and Fu et al. However, Elzen et al. reported no significant difference in exercise and communication with a physician with p-value 0.624 and 0.081 respectively. Lastly, one quasi-experimental design (25) found significant improvement in all the four sub components of the self-management behaviour. Therefore, it appears that majority of the older adults who participated in CDSMP showed significant improvement in exercise and cognitive symptom management than those who did not participate in CDSMP.
Four studies evaluated health service utilization of the participants whereas Elzen et al. did not measure this outcome. There were four sub components of this outcome. These four components included number of visits to general physician, emergency department visits, hospital stays and nights spent in hospital. Lorig et al. reported improvement in healthcare utilization with decrease in the number of hospitalizations (p 0.047) and in the number of nights of hospitalization (p 0.01) in the comparison between the treatment and control group at 6 months. This study showed no improvement in number of visits to general physician and emergency department visits. Fu et al. showed improvement only in hospital stays (p = 0.04) and not found any significance improvement in three remaining components. On the contrary, Swerissen et al. did not find any change in general practitioner visit and emergency department visit and did not examine the hospital stays and nights in hospital. The study of Hong Kong patient (Chan et al., 2011) also found no significance change in number of visits to general physician and emergency department visits, and hospital stay between the treatment and control group. This manifests that there is no change in health service utilization in terms of numbers of visit to general practitioner, emergency department and number in night at hospital for older people who participated in CDSMP. However, it is difficult to conclude the numbers of hospital stay because only two studies measured this component and other studies were unable to examine this data.
In general, the four RCTs and the one quasi-experimental study presented with high to moderate quality evidence in support of the effectiveness of CDSMP for older people with chronic disease. There were few bias in the included studies. Firstly, performance bias due to insufficient reporting of treatment concealment and unable to do blinding. It could be argued, however, that the nature of the intervention might have contributed to this bias. For example, it is not possible to blind or conceal intervention for participants since participants are aware of the intervention when they participate in community based intervention.
Discussion
To the best of our knowledge, this is the first systematic review summarising effectiveness of the CDSMP for community dwelling older people with chronic diseases. Evidence in the literature determined that health care systems that incorporated one or multiple components of Chronic Care Model (CCM) had significant beneficial effects on clinical outcomes and quality of life for patients with chronic diseases. Thus, this systematic review provides the evidence for self-management support which is one of the vital components of CCM and it has been demonstrated that CDSMP is a beneficial program for older people with chronic diseases.
It is believed about the old people that they are considered to be always ill, they receive the aid and depend on others. Older people cannot learn and refuse to change their old behaviour. However, this was not true, older people who participated in the course of CDSM showed significant improvement in their self-efficacy to control chronic diseases and likely to improve their behaviour (particularly exercise) by increasing their use of self-management skills.
It has been suggested that translating theory into intervention can improve clinical effectiveness (28). Lorig who has developed the chronic disease self-management education program has incorporated the self-efficacy theory (29) in this education program. Self-efficacy is the core of this program and is based on the twin assumptions that enhanced self-efficacy improves both health status and health behaviours (18). It has been noted that majority of the included studies demonstrated improvement in self-efficacy among participants. This emphasises that incorporation of theory in education program assisted older people regardless of their culture to develop self-confidence to manage their chronic diseases.
The second outcome was health status. Studies showed significant improvement in health status for older people particularly in self-rated health status and health distress. However, there were inconsistent changes in other components of health status such as pain, fatigue, shortness of breath. It could be because CDSMP includes people with different long-term conditions. Thus, duration and severity of the symptoms such as pain and shortness of breath varies among participants (30). Participants who rated symptoms as minimal at baseline had little room for improvement at follow-up (30). This was supported by one of the excluded studies (31).
Furthermore, improvement was observed in the outcome of health behaviour. Majority of the older adults who participated in CDSMP showed improvement in self-management health behaviour particularly in exercise and cognitive symptom management. Thus, it appears that it is most likely that integration of theory into intervention has given better results in health outcomes.
Table 4.Characteristics of the included studies and participants demographic across the studies
|
Author (Year) Population |
Study Design |
Sample Size |
No of Male or Female (Percentage %) |
Age (Mean Age) |
Mean Education Years |
Outcome Assessed |
|||||||
|
|
|
I |
C |
I |
C |
I |
C |
I |
C |
|
|||
|
|
|
|
|
M |
F |
M |
F |
|
|
|
|
|
|
|
Lorig et al. (1999) USA |
Randomized Controlled Trial |
561 |
391 |
35 |
65 |
36 |
64 |
65.6 |
65.0 |
15 |
15 |
self-efficacy not reported health status health behaviours health service utilization |
|
|
Fu Dongbo et al. (2003) Urban communities in Shanghai, China. |
Randomized controlled Trial |
430 |
349 |
115 |
315 |
108 |
241 |
64.2 |
63.8 |
9.48 |
9.88 |
self-efficacy health status health behaviours health service utilization |
|
|
Swerissen et al. 2006 Greek (G), Italian (I) Vietnamese (V) and Chinese (C), backgrounds living in Victoria, Australia |
Randomized Controlled Trial |
320 G 80 I 73 V 96 C 71 |
154 27 32 64 31 |
12.5 27.4 32.3 36.6 |
87.5 72.6 67.7 63.4 |
11.1 25 20.3 25.8 |
88.9 75 79.7 74.2 |
64.9 68.7 65.6 66.9 |
67.4 69.3 60.4 68 |
7.08 |
6.21 |
self-efficacy health status health behaviours health service utilization |
|
|
Elzen et al. (2007) NetherLands (Dutch) |
Randomized Controlled Trial |
68 |
68 |
36.8 |
66.2 |
36.8 |
58.8 |
68.2 |
68.5 |
Not mentioned |
self-efficacy health status health behaviours health service utilization was not reported |
||
|
Chan et al. (2011) Hong Kong |
Quasi-experimental |
302 |
298 |
23.2 |
76.8 |
17.2 |
82.8 |
72.5 |
76.0 |
4.04 |
3.68 |
self-efficacy health status health behaviours health service utilization |
|
Note: I (Intervention group) & C (Control group)
Table 5. Primary and secondary outcomes
|
Study |
Self-efficacy |
Health Status |
Health Behaviour |
Health Service Utilization |
|
Lorig et al. (1999) |
Did not measure the self-efficacy |
Improvement - Self-rated health (p 0.02) - Health distress (p 0.001) - Fatigue / energy (p 0.003) - Disability (p 0.002) - Social/ role activities (0.0007) No Improvement - Pain/physical discomfort (p 0.27) - Shortness of breath (p 0.56) - Psychological well-being (p 0.1) |
Improvement - Aerobic exercise (p 0.0003) -Stretching and strengthening exercise (p 0.005) -Communication with physician (p 0.006) - Cognitive symptom (p 0.0001) |
Improvement - Hospital stay (p 0.047) - Nights in hospital (p 0.01) No improvement - MD and ER visit (p 0.11) |
|
Fu Dongbo et al. (2003) |
Improvement - Managing symptoms (p 0.001) - Managing disease in general (p 0.001) |
Improvement - Self-rated health (p 0.001) - Health distress (p 0.001) - Pain/physical discomfort (p 0.02) - Disability (p 0.005) - Social/ role activities (p 0.046) - Fatigue (p 0.03) - Shortness of breath (p 0.01) - Depression (p 0.004) No Improvement - illness intrusiveness (p 0.06) - Energy (p 0.93) |
Improvement - Aerobic exercise (p 0.01) - Cognitive symptom (p 0.005) No improvement: -Stretching and strengthening exercise (p 0.07) -Communication with physician (p 0.89) |
Improvement Hospital stay (p 0.04) No improvement: - Physician visit (p 0.72) - Emergency room visit (p 0.44) - Nights in Hospital (p 0.40) |
|
Swerissen et al. (2006) |
Improvement General self-efficacy (p <0.0001) |
Improvement - Self-rated health (p <0.001) - Health distress (p 0.043) - Fatigue (p 0.016) - Pain (p 0.001) - Energy (p <0.001) No Improvement: - Shortness of breath (p 0.67) - Disability (p 0.426) - illness intrusiveness (p 0.076) - Depression (p 0.422) - Social/role activity limitation (p 0.067) |
Improvement - Exercise (p 0.005) - Cognitive symptom (p <0.001) |
No improvement - General practitioner visit (p 0.239) - Specialist visit (p 0.877) - Allied health practitioners visit (p 0.152) - Mental health practitioners visit (p 0.906) - Emergency department visit (p 0.683) |
|
Elzen et al. (2007) |
No improvement General self-efficacy (p 0.555) |
No improvement Measurement: RAND-36 (Zee & Sanderman, 1993) - Physical component (p 0.45) - Mental component (p 0.46) |
No improvement - Exercise (p 0.624) -Communication with physician (p 0.081) |
Not measured |
|
Chan et al. (2011) |
Improvement -Managing symptoms (p <0.0005) -Managing disease in general (p <0.0005) |
Improvement - Self-rated health (p 0.010) - Health distress (p 0.014) - Pain/physical discomfort (p 0.006) - Disability (p 0.058) - Social/ role activities (p 0.004) - Energy (p 0.059) No Improvement - Shortness of breath (p 0.336) - Psychological well-being (p 0.064) - Fatigue (p 0.654) |
Improvement - Aerobic exercise (p 0.005) -Stretching and strengthening exercise (p < 0.001) - Communication with physician (p < 0.001) - Cognitive symptom (p < 0.001) |
No improvement: - Physician visit (p 0.107) - Emergency room visit (p 0.534) - Nights in Hospital (p 0.773) |
Finally, the outcome of health service utilization. This review demonstrated that there was no reduction in health service utilization in terms of numbers of visits to general practitioner, emergency department and number of nights in hospital for older people who participated in CDSMP. However, it was difficult to conclude on the outcome of hospital stay because only two studies measured this component and other studies were unable to examine this data. There were two factors that may have affected the outcome of health service utilization. First, all measures used in these studies were based on self-report and may be compromised by inability to remember the past correctly (especially the exact timing of a physician or ER visit) (32, 33). Secondly, perhaps there were differences in health care systems among different countries or less access to health care services so little or no change was possible (34, 35). For example, in many middle and low income countries patients tend to rely on the heavily subsidised public health care system, and they may be deterred from using private general practitioners. They may rather turn to the emergency room in public hospitals for ad hoc medical problems. In addition, in these countries health care services were not easily available within the community setting. Mostly services are accessible in city centres that need transportation. This might have made difficult for rural communities to access these services with limited economic resources.
Overall, it clearly seems that older people who participated in CDSMP are most likely to improve self-efficacy to manage disease in general and to manage symptoms. Furthermore, elderly people are likely to improve some of their components of health status. Moreover, these people are likely to show significant improvement in health behaviour. However, there is no improvement in some aspects of health service utilization.
It is interesting to note that the outcomes received here are those specified by Lorig (26). They are relevant and appropriate but may not capture the learning associated with all the elements of the program. On the other hand, cost effectiveness and involvement of lay leaders are two important elements that need to be considered for successful implementation of this program.
Cost effectiveness is one of the key factors for decision making to adopt and fund any health care program. In this review, studies included had examined the cost-effectiveness in terms of health services utilization and concluded that there is no improvement in health service utilization in terms of numbers of visit to general practitioner, emergency department and number in night at hospital. However, there are evidences in the literature that have evaluated the program cost-effectiveness from societal perspective. These studies have concluded that CDSMP has probability of being cost-effective. For example, Richardson et al. estimated the costs of CDSMP in England conducting a randomized controlled trial over a 6-month period from a societal perspective. They found that intervention group has a 0.020 Quality-adjusted life years (QALY) gain compared with the control group, and a reduced cost of around 27 pounds per patient. They reported further that when the value of a QALY is 20,000 pounds the CDSMP has a probability of 94% of being cost effective. Although the cost effectiveness in term of health service utilization was not demonstrated, this program assists elderly to be independent and self-manage their health care problems and improves their wellbeing and quality of life (36).
Involvement of volunteer lay leader in CDSMP is another important factor that needs to be considered cautiously before implementing this program as it might effect on the outcome of the participant and program success. Upon the critical examination of the studies it was identified that lay-leader plays essential role in CDSMP. It was observed that the CDSMP program was mostly conducted by the lay-leader who had chronic condition and was specifically trained. The trained lay-leader either paired up with the health professional or another lay tutor. However, the interpretation of who exactly qualifies as a lay-leader in terms of their experience to teach the program and experience of disease was not clearly described in the reviewed studies.
With regard to experience, none of the studies stated the lay leader’s experience level to teach the program and since how many years he/she is suffering from chronic disease. Even though, the teachers were trained specifically for the program arguably, their experience still has significances on how successfully they lead the program. For example, USA lay-leader experiences would be different from Hong Kong lay- leader. This will not only affect the outcomes of the participants; it will also affect the program’s success. The program is considered successful if there is less drop-out of participants from the program and/or the program is sustainable. It seems that it could be the reason, in some studies lay leaders are paired with health professional to provide correct information to the participants so they can act as check and balance for each other (37).
However, effectiveness of lay-led self-management education interventions for chronic conditions compared with health professionals such as doctors or nurses has been documented. A Cochrane Review by Foster et al. assessed the effectiveness of lay-led self-management programs for people with chronic conditions. This review included 17 studies with 7, 442 individuals with chronic conditions such as arthritis, diabetes, hypertension and chronic pain. This review found modest improvement in patients’ confidence to manage their condition and perceptions of their own health (38). There was also increase in the amount of aerobic exercise by participants. There were small improvements in pain, disability, fatigue and depression. From this Cochrane review it appears that there were no major differences in outcomes of the participants associated with who delivered the interventions (38). It can be explained as lay-leader or peer support act as role model for the participants. In a group, when newly diagnosed patient has a problem, lay leader can be asked to offer suggestion who has experience with the disease or treatment (37). Furthermore, it is said that if participants observe that other people in group participating in some sort of exercise and experiencing positive effects then it is more likely that they follow. This is the reason the involvement of lay-leader has great importance in the CDSMP. They lead the course by acting as role models for other participants and enhance their self-confidence to improve health status and change the health behaviour. Thus, it indicates that involvement of a lay leader in healthcare system might be a strategy to tackle the global scarcity of health care workforce. However, volunteer commitment and engagement could influence over all success of the program and this area need caution to scale-up its implementation.
Conclusion
This review concludes that elderly people with chronic disease who have participated in CDSMP are most likely to improve self-efficacy. In addition, they are likely to improve some elements of their health status and health behaviour as opposed to elderly people who have not participated in CDSMP. However, there is no improvement in health service utilization.
This review has a number of strengths. First, it is the only review to examine the group base Stanford’s model of generic CDSMP and not in combination of other disease-specific self-management education interventions. Second, it includes the explicit eligibility criteria and conducts a comprehensive search to identify eligible studies. Third, it assesses the 20 different outcomes. Another important strength of this review is that this includes study population from different parts of the world which would help in the generalisation of the study findings.
Study limitations
This systematic review is not without its own limitations. Firstly, meta-analysis would have been the best approach for synthesising the results in order to get a pooled estimate of intervention effects. However, due to many different targeted outcomes, difference in methods of evaluation in different sub outcomes and difference in reporting of outcome analysis, meta-analysis was considered inappropriate. Second, this review has considered participant mean age of 60 years or above instead of investigated specifically 60 year or above age group. Because, a very few studies have investigated the intervention specifically for 60 years and above. Therefore, the inclusion criteria were amended to include those studies that have documented participant mean age 60 years or above and FU Dongbo et al. was included in review. This avoid inclusion bias for excluding relevant studies (16) and to reduce the possibility of reviewer selection on the basis of studies result (17). Third, this review has analysed only six months follow-up RCTs that could be too short period to observe the improvement in chronically ill older patients. Thus, extended follow-up will be useful to confirm that the skills attained by elderly people are incorporated into their daily lives. This will enable us to determine the program’s sustainability that the beneficial effects are maintained for long duration, and have impact in real world setting.
In a nutshell, this review recommends policy makers to incorporate the CDSMP as a part of usual care. Government and other stakeholders from other health care organizations must understand the health care provision for the elderly population and prioritise services towards the best approach of CDSMP. To emphasise the service development for CDSMP for elderly people’s health care, a work group can be formed. This work group includes members from a non-profit health care organization and the public and private health sectors. They could discuss the issue of elderly population’s health care provision and influence policy makers to incorporate the CDSMP as a part of usual care. Introduction of CDSMP has a great potential to enhance the wellbeing of the elderly population.
Conflicts of interest
None of the authors have a conflict of interest regarding any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work.
Acknowledgements
We would like to thank Dr Linda East for her contribution in supervising and reviewing this systematic review as thesis submitted in University of Nottingham.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors Contribution
Conception of idea: KM
Data Extraction and Analysis: KM and HM
Manuscript Writing Initial Draft: KM
Manuscript Reviewing and Formatting: HM
All the authors have read the manuscript and approved the final version.
References
1. Anette B, Sylvie R-D, Axel Z, Maurits B, Adrie D, Miriam L. Special issue on healthcare: Healthy ageing and the future of public healthcare systems. Belgium: European Commission; 2009.
2. Government of Pakistan. Provisional Summary Results of 6th Population and Housing Census [Internet]. Pakistan: Pakistan Bureau of Statistics; 2017. Available from: http://www.pbs.gov.pk/content/provisional-summary-results-6th-population-and-housing-census-2017-0
3. Lloyd-Sherlock P. Epidemiological change and health policy for older people in developing countries: some preliminary thoughts. Ageing Horizons. 2005; 2: 21-24.
4. World Health Organization. The world health report 2002: reducing risks, promoting healthy life [Internet]. World Health Organization; 2002. Available from: https://www.who.int/whr/2002/en/whr02_en.pdf?ua=1
5. World Health Organization. World report on ageing and health. World Health Organization [Internet]. World Health Organization; 2015. Available from: https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf?sequence=1
6. Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME, et al. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. The Lancet. 2018; 392(10152): 1072-88.
7. World Health Organization. Noncommunicable diseases country profiles 2014 [Internet]. World Health Organization; 2014. . Available from: https://apps.who.int/iris/bitstream/handle/10665/128038/9789241507509_eng.pdf;jsessionid=5DC159DE6A62D4BFFC38663D07CADF87?sequence=1
8. Najam A, Bari F. Pakistan National Human Development Report. Unleashing the Potential of a Young Pakistan. Islamabad: UNDP. 2017.
9. Sabzwari SR, Azhar G. Ageing in Pakistan—a new challenge. Ageing International. 2011; 36(4): 423-7.
10. Baig L, Hasan Z, Iliyas M. Are the elderly in Pakistan getting their due share in health services? Results from a survey done in the peri-urban communities of Karachi. The Journal of the Pakistan Medical Association. 2000; 50(6): 192-6.
11. Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Bandura A, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001; 39(11): 1217-23.
12. Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, et al. Meta-analysis: chronic disease self-management programs for older adults. Annals of Internal Medicine. 2005; 143(6): 427-38.
13. Porritt K, Gomersall J, Lockwood C. JBI's systematic reviews: study selection and critical appraisal. The American Journal of Nursing. 2014; 114(6): 47-52.
14. Webb C, Roe B. Reviewing research evidence for nursing practice: Systematic reviews. John Wiley & Sons; 2008.
15. Holopainen A, Hakulinen-Viitanen T, Tossavainen K. Systematic review–a method for nursing research. Nurse Researcher. 2008; 16(1): 72-83.
16. Leandro G. Meta-analysis in Medical Research: The handbook for the understanding and practice of meta-analysis: John Wiley & Sons; 2008.
17. Torgerson CJ. Publication bias: the achilles’heel of systematic reviews? British Journal of Educational Studies. 2006; 54(1): 89-102.
18. Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effective Clinical Practice: ECP. 2001; 4(6): 256-62.
19. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology. 2009; 62(10): 1-34.
20. Joanna Briggs Institute. Meta-analysis of statistics: Assessment and review instrument (JBI MASTARI). Adelaide: Joanna Briggs Institute. 2006;20032007.
21. Lorig KR, Sobel DS, Stewart AL, Brown Jr BW, Bandura A, Ritter P, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Medical Care. 1999; 37(1): 5-14.
22. Fu D, Fu H, McGowan P, Shen Y-e, Zhu L, Yang H, et al. Implementation and quantitative evaluation of chronic disease self-management programme in Shanghai, China: randomized controlled trial. Bulletin of the World Health organization. 2003; 81(3): 174-82.
23. Swerissen H, Belfrage J, Weeks A, Jordan L, Walker C, Furler J, et al. A randomised control trial of a self-management program for people with a chronic illness from Vietnamese, Chinese, Italian and Greek backgrounds. Patient Education andCounseling. 2006; 64(1-3): 360-8.
24. Elzen H, Slaets JP, Snijders TA, Steverink N. Evaluation of the chronic disease self-management program (CDSMP) among chronically ill older people in the Netherlands. Social Science & Medicine. 2007; 64(9): 1832-41.
25. Chan WL, Hui E, Chan C, Cheung D, Wong S, Wong R, et al. Evaluation of chronic disease self-management programme (CDSMP) for older adults in Hong Kong. The Journal of Nutrition, Health & Aging. 2011; 15(3): 209-14.
26. Lorig K, Stewart A, Ritter P, Gonzalez V, Lynch J, Laurent D. Outcome measures for health education and other health care interventions. Sage; 1996.
27. Bosscher RJ, Smit JH. Confirmatory factor analysis of the general self-efficacy scale. Behaviour Research and Therapy. 1998; 36(3): 339-43.
28. Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. 2th ed. San Francisco; John Wiley & Sons; 2008.
29. Bandura A. Self-efficacy in changing societies. UK: Cambridge University Press; 1997.
30. Gallagher R, Donoghue J, Chenoweth L, Stein-Parbury J. Self-management in older patients with chronic illness. International Journal of Nursing Practice. 2008; 14(5): 373-82.
31. Reeves D, Kennedy A, Fullwood C, Bower P, Gardner C, Gately C, et al. Predicting who will benefit from an expert patients programme self-management course. The British Journal of General Practice. 2008; 58(548): 198-203.
32. Groves RM, Fowler Jr FJ, Couper MP, Lepkowski JM, Singer E, Tourangeau R. Survey methodology. 2th ed. Canada; John Wiley & Sons; 2009.
33. Ritter PL, Stewart AL, Kaymaz H, Sobel DS, Block DA, Lorig KR. Self-reports of health care utilization compared to provider records. Journal of Clinical Epidemiology. 2001; 54(2): 136-41.
34. Yukawa K, Yamazaki Y, Yonekura Y, Togari T, Abbott FK, Homma M, et al. Effectiveness of chronic disease self-management program in Japan: preliminary report of a longitudinal study. Nursing & Health Sciences. 2010; 12(4): 456-63.
35. Williams TR. A cultural and global perspective of United States health care economics. Seminars in Radiation Oncology. 2008; 18(3): 175-85.
36. Richardson G, Kennedy A, Reeves D, Bower P, Lee V, Middleton E, et al. Cost effectiveness of the Expert Patients Programme (EPP) for patients with chronic conditions. Journal of Epidemiology & Community Health. 2008; 62(4): 361-7.
37. Lorig KR, Ritter PL, González VM. Hispanic chronic disease self-management: a randomized community-based outcome trial. Nursing Research. 2003; 52(6): 361-9.
38. Foster G, Taylor SJ, Eldridge S, Ramsay J, Griffiths CJ. Self-management education programmes by lay leaders for people with chronic conditions. The Cochrane Database of Systematic Reviews. 2007; 4: CD005108.
Received: 2019/10/10 | Accepted: 2020/06/21 | Published: 2020/06/27
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








