BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ehj.ssu.ac.ir/article-1-218-en.html
Emine Ekici*1, Nursel Vatansever 2, Merve Çolak 1,3, Ezgi Hasret Kozan 1,3
- Department of Nursing, Faculty of Health Sciences, Uskudar University, İstanbul, Turkey
- Department of Surgical Diseases Nursing, Faculty of Health Sciences, Uludağ University, Bursa, Turkey
- Department of Public Health Nursing, Istanbul University-Cerrahpasa Florence Nightingale Faculty of Nursing, İstanbul, Turkey
Article history
Received 11 Jan 2021
Accepted 4 Apr 2021
A B S T R A C T
Introduction: The most common nutritional problem observed among the aged is malnutrition. The study was conducted as methodological research to evaluate the validity and reliability of the Turkish Self Mini Nutritional Assessment Scale (Self-MNA) among Turkish elderly people.
Methods: Data were collected from 131 aged individuals with the Sociodemographic Information Form, Mini Nutritional Assessment long-form (MNA), Mini Nutritional Assessment short-form (MNA-SF) and Self-MNA. In the study, test-retest, parallel form methods, lower 27%-upper 27% discrimination, ROC and correlation analysis were used to evaluate the validity and reliability of the scale. The scale was translated and then the final version was created by the views of three experts. A correlation analysis was conducted between MNA, MNA-SF and Self-MNA which are used as parallel forms.
Results: No statistically significant difference was found between test-retest scores of Self-MNA scores for reliability (p > 0.05). Positive relationships were found between Self-MNA and MNA and MNA-SF. Self-MNA scores of the upper 27% group were significantly higher than the Self-MNA scores of the lower 27% group. The appropriate cut-off value of Self MNA is determined as 12. Self-MNA scores below 12 points indicate that there may be a risk of malnutrition. The areas under the ROC curves (AUC = 0.718) were statistically significant (p < 0.05). At the cut-off value, the sensitivity is determined to be 75 and the specificity is 56.63.
Conclusion: Self-MNA is a valid and reliable tool for screening the malnutrition status of the aged in Turkey.
Keywords: Nutrition Assessment, Aged, Malnutrition, Validity
The most common nutritional problem observed among the elderly is malnutrition. Unbalanced nutrition in the elderly can cause chronic diseases, such as cancer, cardiovascular diseases, hypertension, and diabetes mellitus (2). Although malnutrition is not a natural component of aging, every elderly individual is at risk of malnutrition because of the physiological, psychological, and social risk factors (1, 3, 4). Malnutrition in the elderly is often observed as protein-energy malnutrition (2, 5, 1).
A retrospective analysis of data collected from older people from 12 countries revealed that the overall prevalence of malnutrition was approximately 23%. The highest prevalence of malnutrition was observed in rehabilitation settings (50.5%), followed by hospitals (38.7%), nursing homes (13.8%), and community (5.8%) (6). Based on the Academic Geriatrics Society’s project on nutritional status assessment in Turkish nursing homes and daycare centers, the overall rate of malnutrition risk was noted to be 38.3%, and the rate of malnutrition was 11.9% (7). Factors like physiological changes of aging, acute and chronic diseases, dental and oral health problems, polypharmacy, economic problems, inability to shop alone, inability to prepare meals, and inability to eat play a crucial role in the deterioration of nutritional status in the elderly (2,3). Notably, unprevented malnutrition in the elderly can cause loss of autonomy, decrease in quality of life, increase in hospital admissions, increase in geriatric syndromes, prolongation of hospital stay, infections, delays in wound healing, gait disorders, falls and fractures, and untimely deaths. Therefore, every elderly individual should be evaluated regarding malnutrition (8-10). Per the European Society of Clinical Nutrition and Metabolism guidelines, all individuals older than 65 years are recommended to be routinely screened for nutritional status (11).
It is recommended to adopt a health protection approach in nutritional interventions (2). This approach can be used in the early diagnosis and prevention of malnutrition in the elderly. Moreover, nurses play an active role in protecting, maintaining, and improving the health of the individual, family, and society. Nurses are involved in determining the risk of malnutrition, as well as planning and implementing interventions in the elderly (9).
Depending on the nutritional status of elderly individuals, various screening tools are used to identify the elderly with malnutrition or those at risk of malnutrition. Notably, screening tests facilitate the early identification of nutritional behaviors, as well as the risks and protective factors associated with nutritional status rather than detecting the actual nutritional level (12, 13). Between 1998 and 2002, 71 screening tests were developed, and 21 of these were noted to be applicable for elderly individuals. Mini Nutritional Assessment (MNA) (14) is one of the significant nutritional screening tools for the elderly that has excellent reliability and validity and is used frequently (15, 16). It is recommended to use MNA to diagnose nutritional status in the elderly in the home environment (17). An individual’s self-assessment of nutritional status and referral to the specialist when necessary may enable early diagnosis and prevention of malnutrition. For this purpose, Self-MNA has developed in 2013 (5) and its validity has been studied by other researchers (18-19). Nevertheless, no screening tool was available in our country that could help the elderly to evaluate their nutritional status themselves.
This study aimed to evaluate the validity and reliability of Self-MNA among the elderly population of Turkey.
Methods
Study design
This study was designed to methodologically evaluate the validity and reliability of the Turkish version of Self-MNA.
Instruments
Data were collected using Sociodemographic Data Collection Form, MNA (14), MNA-SF (20), and Self-MNA (5).
Sociodemographic Data Collection Form: This is a questionnaire consisting of 18 questions regarding sociodemographic and general health status (chronic illness, frequency of physical activity, appetite, chewing difficulty).
Mini Nutritional Assessment Test - Long and Short Form: MNA was developed in 1994 in collaboration with the University of Toulouse, New Mexico School of Medicine, and the Nestle Research Center of Switzerland (3). MNA is considered to be a valid instrument for detecting the risk of malnutrition, as well as detecting malnutrition in geriatric patients. MNA starts with six screening questions (questions A-F1/F2), which are a maximum of 14-point MNA-SF. These questions are related to the patient’s food intake, weight loss, mobility, psychological stress or acute illness, depression or memory problems, and the determination of the body mass index (BMI). Notably, measuring calf circumference has been proven to be appropriate if BMI measurement is impossible. If less than 12 points are obtained as a result of this questioning, it is recommended to continue the other questions (questions G-S). These questions relate to residential status, drug use, pressure sores or skin inflammation, food ingestion and protein and fluid intake, the patient’s view of nutrition and health, and some extra anthropometric measurements, which form the final MNA score. A score of 23.5 indicates an adequate nutritional status (3). The validity of the Turkish versions of MNA and MNA-SF was conducted in 2013 (21).
Self-Mini Nutrition Diagnosis Scale (Self-MNA): A study was conducted in 2013 to validate Self-MNA that can be used by elderly individuals to self-assess their nutritional status (5). Evaluation parameters were the general health status of the elderly, mobility, nutritional status, and anthropometric measurements (weight loss, BMI, calf circumference). Self-MNA consists of seven questions. Only one of the last two questions, questions 6 and 7, are answered according to preference. The diagnostic scale receives a maximum of 14 points and a minimum of 0 points. A score of 12-14 indicates normal nutritional status, 8-11 points indicate malnutrition risk, and 0-7 points indicate malnutrition. This form can be filled in either by the elderly person or the caregiver.
Participants
The participants comprised of 131 individuals, older than 65 years old, who applied to the geriatric outpatient clinic of Istanbul University – Istanbul Faculty of Medicine between May 2018 and December 2018. Overall, 65.6% (n = 86) of the participants were women and 34.4% (n = 45) of them were men, with a mean age of 72.74 years.
Data collection
The preliminary application of the study was performed with 15 individuals above 65 years. The study included patients with no communication disabilities, who could understand and answer questions, who did not have psychiatric and cerebral problems per the DSM-IV criteria, and who accepted to participate in the study. Data were collected in two stages. In the first stage, each elderly individual was given the informed consent and Self-MNA forms by the researchers to answer the questions in a self-report method. In the second stage, the height and weight of the individuals were measured using an anthropometry kit consisting of a calibrated weighing scale and measuring tape. The MNA and MNA-SF scales were filled during a face-to-face interview. The measurements were collected in a special environment (examination room) where the elderly were weighed without shoes and wearing only light clothing.
Translation of the Self-MNA scale
The items of the scale were first translated from English to Turkish and then vice versa by three experts. The translations were compared by two researchers who were proficient in both English and the concepts of the research, and the most appropriate translation text was obtained. The results were evaluated by three experts for the face validity of the obtained scale, and it was put into the final form.
Data analyses
The data obtained from the study were analyzed using SPSS 22.0 and MedCalc program. The data were expressed as numbers, percentages, mean values, and standard deviation values in descriptive statistical methods. Reliability and validity were analyzed using test-retest, parallel form analysis, lower 27%-upper 27% discrimination, ROC analysis and correlation analysis to determine the relationship between the measurements. The t-test was used to compare scale scores according to descriptive characteristics and the continuous quantitative data between two independent groups. The one-way ANOVA test was used to compare the continuous quantitative data between more than two independent groups.
Ethical considerations
Necessary permission was obtained via e-mail from the authors to adapt the Self-MNA scale to Turkish. Permission, bearing the number B.08.6.YOK.2.US.0.05.0.06/2018/734, was obtained from the Non-Interventional Clinical Research Ethics Committee of Uskudar University Institute of Health Sciences to conduct the study. Also, permission was obtained from Istanbul University - Istanbul Faculty of Medicine. We paid special care to the principle of volunteering in participation in the study and explained the purpose of the study, our expectations, and legal rights to the patients making up the study group. Afterward, written and verbal informed consent of the patients was obtained.
Results
- Sociodemographic characteristics, general health status, and nutritional characteristics of participants
It was found that 65.6% (n = 86) of the participants do not smoke, 88.5% (n = 116) of them do not use alcohol, and 67.2% (n = 88) of them are physically inactive.
2. Validation of the scale
Test-retest and parallel form analyzes were performed to determine the reliability of the Self-MNA scale, and ROC analysis and item difficulty analysis were performed to test its validity. Since the scale includes dichotomous responses, Cronbach Alpha was not used to determine reliability (22). Findings related to the analyzes are stated in the same order. In the Self-MNA test-retest analysis performed to determine the reliability, no statistically significant difference was found between the scores (r = 0.720 p = 0.232). In the reliability analysis of the scale, as a result of the correlation analysis made with the MNA and MNA-SF scores used in parallel form r = 0.619 positive correlation (p = 0.000) between MNA and Self-MNA, r = 0.799 positive correlation between MNA-SF and Self-MNA (p = 0.000), and r = 0.755 positive correlation between MNA-SF and MNA (p = 0.000) was found.
Overall, 48 (36.64%) positive and 83 (63.36%) negative values were noted for MNA status. In the ROC analysis performed for the validity of the scale, areas under the ROC curves (AUC = 0.718) were found to be statistically significant (p < 0.05) (Figure 1). The optimum cut-off value was ≤ 12. Sensitivity at the cut-off point was 75, and specificity was determined as 56.63. Youden index was found to be J = 0.316 (0 < J = 0.316 < 1) (Tables 1 and 2).Criterion values and coordinates of the ROC curve [Show].
In the Item Difficulty Analysis, the Self-MNA scores of the upper 27% (x̄ = 14.000) were found to be significantly higher than the Self-MNA scores of the lower 27% (x̄ = 8.971) (t (68) = −17.437; p = 0.000) (Table 3).
Table 1. Self MNA ROC curve findings
| Areas under the ROC curve (AUC) | 0.718 |
| Standard Error | 0.0467 |
| 95% confidence interval | 0.632 - 0.793 |
| Z statistics | 4.667 |
| Significance level P (Area = 0.05) | < 0.0001 |
| Youden index J | 0.3163 |
| Associated criterion | ≤ 12 |
| Sensitivity | 75.00 |
| Specificity | 56.63 |
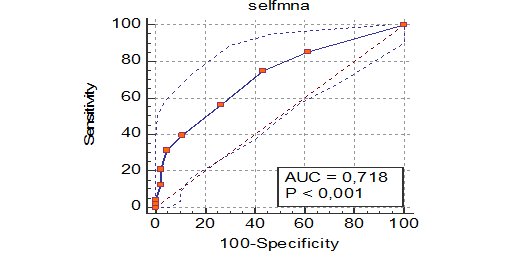
Figure 1. Self MNA ROC Curve
According to the MNA form, 63.4% (n = 83) of the participants were normal, 34.4% (n = 45) were at the risk of malnutrition, and 2.3% (n = 3) of them were malnourished. According to MNA, 68.7% (n = 90) of the participants were normal, 28.2% (n = 37) of them were at risk of malnutrition, and 3.1% (n = 4) of them were malnourished. According to Self-MNA, 65.6% (n = 86) of the participants were normal, 29.8% (n = 39) of them were at risk of malnutrition, and 4.6% (n = 6) of them were malnourished. According to Self-MNA, 37.4% (n = 49) of the participants scored below 12, and 62.6% (n = 82) of them scored 12 and above (Table 4).
3. Comparison of MNA scores by using descriptive characteristics
No significant difference was observed in the mean scores of MNA, MNA-SF, Self-MNA of the elderly based on sex, educational status, presence of chronic disease, diet, drug use, smoking status, daily meal (main meals and snacks) skipping status, chewing-swallowing difficulties, and tooth loss (p > 0.05).
When the mean scores of MNA, MNA-SF, and Self-MNA of the elderly were examined, the MNA scores (x = 24.872) of those who do physical activity were observed to be higher than the MNA scores (x = 23,739) of those who did no physical activity (t = 2.188; p = 0.03).
Notably, MNA-SF and Self-MNA mean scores of the elderly did not differ significantly based on the physical activity status (p > 0.05).
Mean MNA scores of the elderly were significantly different based on the appetite status (F = 5.280; p = 0.006). The MNA scores of those with good appetite status were higher than those with poor appetite status (p < 0.05). Moreover, the MNA scores of those with moderate appetite were higher than those with poor appetite (p < 0.05).
Self-MNA mean scores of the elderly exhibited significant difference based on the appetite status (F = 5.414; p = 0.006). The Self-MNA scores of those with good appetite status were higher than those with poor appetite status (p < 0.05). Self-MNA scores of those with moderate appetite were higher than those with poor appetite (p < 0.05).
The MNA-SF scores of the elderly did not differ significantly based on the appetite status variable (p > 0.05).
Discussion
In this study, the validity and reliability of Self-MNA in Turkish was investigated. Accordingly, the optimum cut-off value of Self-MNA was determined as ≤ 12. In the ROC analysis, the areas under the ROC curves (AUC = 0.718) were noted to be statistically significant (p < 0.05). Sensitivity at the cut-off point was determined as 75 and the specificity as 56.63. Youden index was found to be J = 0.316 (0 < J = 0.316 < 1). According to this finding, 12 points can be used as a cut-off point in the Self-MNA tool. Values below 12 points on Self-MNA would indicate malnutrition or risk of malnutrition. Screening tools that assess nutritional status are typically short and time-consuming. These tools determine malnutrition and the risk of malnutrition. In individuals who are noted to be malnourished or at risk of malnutrition, the underlying reasons, the severity, and the type of malnutrition should be evaluated by an expert (3). Based on this information, Self-MNA can also be used by the individual himself or his relative to assess the risk of malnutrition.
Three international studies on Self-MNA were noted. Huhman MB et al. determined that Self-MNA is a reliable tool that can be used for nutrition screening of elderly individuals in the community. In this study, the agreement between Self-MNA and MNA-SF was observed to be 99% (Self-MNA sensitivity: 99%, specificity: 98%, false-negative rate: 1%, false positive rate: 2%) (5). The reason for the lower sensitivity and specificity values in this study was considered to be probably from the differences in the parallel form used.
| Criterion | Sensitivity | 95% CI | Specificity | 95% CI | +LR | -LR |
| < 4 | 0.00 | 0.0 - 7.4 | 100.00 | 95.7 - 100.0 | 1.00 | |
| ≤ 4 | 2.08 | 0.05 - 11.1 | 100.00 | 95.7 - 100.0 | 0.98 | |
| ≤ 6 | 4.17 | 0.5 - 14.3 | 100.00 | 95.7 - 100.0 | 0.96 | |
| ≤ 7 | 12.50 | 4.7 - 25.2 | 97.59 | 91.6 - 99.7 | 5.19 | 0.90 |
| ≤ 8 | 20.83 | 10.5 - 35.0 | 97.59 | 91.6 - 99.7 | 8.65 | 0.81 |
| ≤ 9 | 31.25 | 18.7 - 46.3 | 95.18 | 88.1 - 98.7 | 6.48 | 0.72 |
| ≤ 10 | 39.58 | 25.8 - 54.7 | 89.16 | 80.4 - 94.9 | 3.65 | 0.68 |
| ≤ 11 | 56.25 | 41.2 - 70.5 | 73.49 | 62.7 - 82.6 | 2.12 | 0.60 |
| ≤ 12 | 75.00 | 60.4 - 86.4 | 56.63 | 45.3 - 67.5 | 1.73 | 0.44 |
| ≤ 13 | 85.42 | 72.2 - 93.9 | 38.55 | 28.1 - 49.9 | 1.39 | 0.38 |
| ≤ 14 | 100.00 | 92.6 - 100.0 | 0.00 | 0.0 - 4.3 | 1.00 |
Table 3. Differentiation status of self MNA scores by lower 27% and upper 27% groups
| Groups | Lower 27% (n = 35) | Upper 27% (n = 35) | t | SD | p | ||
| Mean | SD | Mean | SD | ||||
| Self MNA | 8,971 | 1,706 | 14,000 | 0,000 | -17,437 | 68 | 0,000* |
| Independent groups T-Test *p < 0,05 | |||||||
Table 4. Distribution of groups according to MNA scales
| Groups | Frequency (n) | Percent (%) |
| MNA group | ||
| Normal nutrition | 83 | 63.4 |
| At-risk of malnutrition | 45 | 34.4 |
| Malnourished | 3 | 2.3 |
| MNA short form group | ||
| Normal nutrition | 90 | 68.7 |
| At-risk of malnutrition | 37 | 28.2 |
| Malnourished | 4 | 3.1 |
| Self MNA group | ||
| Normal nutrition | 86 | 65.6 |
| At-Risk of malnutrition | 39 | 29.8 |
| malnourished | 6 | 4.6 |
| Self MNA group (new grouping) | ||
| Under 12 | 49 | 37.4 |
| 12 and above | 82 | 62.6 |
A study conducted by Donini et al. (2018) observed that participants had difficulty in filling the Self-MNA, and 30% had a 30-minute test-filling time (19). In our study, it was observed that some elderly individuals had difficulty filling out forms. In such situations, the elderly may require the caregiver’s assistance.
The aim of the third study by the Moore et al. Meals on Wheels program was to compare the results of Self-MNA with the MNA-SF results among a sample of home-bound older adults newly enrolled in the Meals on Wheels program. The results showed that the Self-MNA screening tool was impractical for this example, as evidenced by the low completion rates. Less than 80% filled the front of the form on the first attempt, and only 40% recorded a final screening score on the back of the form. The authors conclude that to increase the usability of Self-MNA among older adults, it may be necessary to change instructions and format to improve clarity (23). A similar problem was experienced by several participants in this study when filling out the questionnaire. However, these difficulties experienced by the elderly were solved with the support of caregivers.
It is of great importance for the elderly population to be able to self-evaluate at home and determine their health needs, especially when access to health services is limited, such as in the current pandemic situation. In the US, nearly one-third of adult respondents reported having delayed or avoided routine medical care, which might reflect adherence to community mitigation efforts such as stay-at-home orders, temporary closures of health facilities, or additional factors. However, if routine care avoidance were to be sustained, adults could miss opportunities for management of chronic conditions, receipt of routine vaccinations, or early detection of new conditions, which might worsen outcomes (24).
It is recommended that individuals in the pandemic, especially those over the age of 65, who are in the risk group, should follow a balanced diet and daily health monitoring, as well as general prevention measures (25). In pandemic conditions, Self- MNA can be effective for the elderly to be aware of the risks related to malnutrition and to consult an expert.
Conclusions
Changes in physiological, psychological, life behaviors, and social factors observed in the increasing elderly population worldwide have led to inadequate and unbalanced nutrition problems. Therefore, it is recommended that all individuals older than 65 years old to be nutritionally screened. Self-MNA can be used by the individuals themselves or by their relative to assess the risk of malnutrition and Self-MNA is valid for screening elderly individuals in Turkey.
Study limitations
This study included patients who had been admitted spontaneously to the geriatric clinic between the specified dates. Nevertheless, it is recommended that Self-MNA be applied in a more comprehensive sample group.
Conflict of interest
The authors of this paper have no conflicts of interest.
Authors’ contributions
All authors contributed extensively to the work presented in this manuscript. We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed.
References
1. Kansal D, Baliga SS, Kruthika K, Mallapur MD. Nutritional assessment among elderly population of rural Belagavi: a cross-sectional study. International Journal Med Science Public Health. 2016; 5(7): 1496-9.
2. Aslan D, Sengelen, M, Bilir N. Nutritional problems and approaches in old age [Internet]. Ankara: GERIATRIC ASSOCIATION; 2008. [Turkish] [cited 2 Dec 2021]; Available from: https://www.huzurevleri.org.tr/docs/Yaslilik_Doneminde_Beslenme_Sorunlari_ve_Yaklasimlar.pdf.
3. Arıogul S. Malnutrition guidelines for the elderly: the importance of malnutrition [Internet]. Ankara: Academic Geriatrics Association; 2013. [Turkish] [cited 11 Dec 2021]; Available from: http://www.akademikgeriatri.org/files/thn-kitap.pdf.
4. Baz S, Ardahan M. Malnutrition in the elderly, nursing approaches. Balikesir Health Sciences Journal. 2016; 5(3): 147-53. [Turkish]
5. Huhmann MB, Perez V, Alexander DD, Thomas DR. A self-completed nutrition screening tool for community-dwelling older adults with high reliability: A comparison study. The Journal of Nutrition, Health & Aging. 2013; 17(4): 339-44.
6. Kaiser MJ, Bauer JM, Rämsch C, Uter W, Guigoz Y, Cederholm T, et al. Frequency of malnutrition in older adults: a multinational perspective using the Mini Nutritional Assessment. Journal of the American Geriatrics Society. 2010; 58(9): 1734-8.
7. Cankurtaran M, Sake B, Sahin S, Varli M, Doventas A, Balam Doğu Yavuz B, et al. Turkish nursing homes and care homes nutritional status assessment project (THN-malnutrition). European Geriatric Medicine. 2013; 4(5): 329-34.
8. Saka B, Kaya O, Ozturk GB, Erten N, Karan MA. Malnutrition in the elderly and its relationship with other geriatric syndromes. Clinical Nutrition. 2010; 29(6): 745–8.
9.Ozgun Basıbuyuk G, Ayremlou P, Nourı Saeıdlou S, Çinar Z, Ay F, Bektas Y, et al. Evaluation of malnutrition among elderly people living in nursing homes by mini nutritional assessment short form (MNA-SF) in Turkey. MAEDICA – a Journal of Clinical Medicine. 2019; 14(1): 38-44.
10. Bauer JM, Kaiser MJ, Anthony P, Guigoz Y, Sieber CC. The mini nutritional assessment: it's history, today's practice, and future perspectives. Nutrition in Clinical Practice. 2008; 23 (4): 388-96.
11.Volkert D, Beck AM, Berry E, Cederholm T, Cruz-Jentoft A, Goisser S, et al. ESPEN guidelines on clinical nutrition and hydration in geriatrics. Clinical Nutrition. 2019; 38(1): 10-47.
12. Bauer JM, Kaiser MJ, Sieber CC. Evaluation of nutritional status in older persons: nutritional screening and assessment. Current Opinion in Clinical Nutrition & Metabolic Car. 2010; 13(1): 8–13.
13. Ulger Z, Halil M, Kalan I, Balam Doğu Yavuz B, Cankurtaran M, Güngör E, et al. Comprehensive assessment of malnutrition risk and related factors in a large group of community-dwelling older adults. Clinical Nutrition. 2010; 29(4): 507-11.
14. Guigoz Y, Vellas B, Garry PJ. The mini nutritional assessment: MNA. Nutrition in the elderly In: Vellas BJ, Guigoz Y, Garry PJ, Albarede JL, editors. Mini nutritional assessment: a practical assessment tool for grading the nutritional status of elderly patients. Paris: Serdi Publishing Company; 1997.p.15-60.
15. Green SM, Watson R. Nutritional screening and assessment tools for older adults: literature review. Journal of Advanced Nursing. 2006; 54(4): 477-90.
16. Phillips MB, Folley AL, Bernard R, Isenring EA, Miller MD. Nutritional screening in community-dwelling older adults: a systematic literature review. Asia Pacific Journal of Clinical Nutrition. 2010; 19(3): 440-9.
17. Kozakova R, Zelenikova R. Assessing the nutritional status of the elderly living at home. European Geriatric Medicine. 2014; 5 (6): 377-81.
18. Donini LM, Marrocco W, Morrocco C, Lenzi A. Validity of the self- mini nutritional assessment (Self-MNA) for the assessment of nutritional risk. A cross-study study conducted in general practice. The Journal of Nutrition Health and Aging. 2017; 22(1): 44-52.
19. Power L, Mullally D, Gibney E. R, Clarke M, Visser M, Volkert D, et.al. A review of the validity of malnutrition screening tools used in older adults in community and healthcare settings–A MaNuEL study. Clinical Nutrition ESPEN. 2018; 24: 1-13.
20. Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). The Journal of Gerontology A Biological Sciences and Medical Sciences. 2001; 56(6): M366-72.
21. Sarikaya D. Mini nutritional evaluation in geriatric patients validity of long and short (mna-sf) form of (mna) test [MSc thesis]. Ankara: Hacettepe University, Faculty of Medicine; 2013.
22. Quansah, F. The use of cronbach alpha reliability estimate in research among students in public universities in Ghana. African Journal of Teacher Education. 2017; 6(1): 56-64.
23. Moore BE, Friedman BJ, Crixell SH: Usability of the Self-Mini nutritional assessment among older adults receiving home-delivered meals in Texas. Family & Consumer Sciences Research Journal. 2015; 44(2): 159–71.
24. Czeisler MÉ, Marynak K, Clarke KE, Salah Z, Shakya I, Thierry JM, et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States. Morbidity and Mortality Weekly Report. 2020; 69(36): 1250.
25. Cadirci D, Kocakoglu Ş. Risk groups and prevention methods in coronavirus pandemic. Clinical Medicine Family Medicine. 2020; 12(2), 62-8. [Turkish]
Received: 2021/01/11 | Accepted: 2021/04/4 | Published: 2021/06/27
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |