Volume 7, Issue 2 (December 2021)
Elderly Health Journal 2021, 7(2): 58-64 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Soleimanpour H, Abbasian M, Sarbazi E, Paknezhad S P, Jalilvand H, Masoudi N, et al . Predictors of Delay in Seeking Post-Exposure Prophylaxis in Older Adults with Animal Bite Injuries: A Population-Based Study. Elderly Health Journal 2021; 7 (2) :58-64
URL: http://ehj.ssu.ac.ir/article-1-242-en.html
URL: http://ehj.ssu.ac.ir/article-1-242-en.html
Hassan Soleimanpour 
 , Mehdi Abbasian
, Mehdi Abbasian 
 , Ehsan Sarbazi *
, Ehsan Sarbazi * 

 , Seyed Pouya Paknezhad
, Seyed Pouya Paknezhad 
 , Hadi Jalilvand
, Hadi Jalilvand 
 , Nazanin Masoudi
, Nazanin Masoudi 
 , Hosein Azizi
, Hosein Azizi 
 , Zahra Khalili
, Zahra Khalili 


 , Mehdi Abbasian
, Mehdi Abbasian 
 , Ehsan Sarbazi *
, Ehsan Sarbazi * 

 , Seyed Pouya Paknezhad
, Seyed Pouya Paknezhad 
 , Hadi Jalilvand
, Hadi Jalilvand 
 , Nazanin Masoudi
, Nazanin Masoudi 
 , Hosein Azizi
, Hosein Azizi 
 , Zahra Khalili
, Zahra Khalili 

Road Traffic Injury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran , ehsansarbazi20@gmail.com
Full-Text [PDF 1169 kb]
(624 Downloads)
| Abstract (HTML) (1679 Views)
Introduction
Animal bites is one of the major health threats specially in rabies endemic areas, because in every bite is potentially a suspected exposure (1). Rabies is a viral infection that affects mammals' central nervous systems and is fatal once symptoms appear (2). The two main mechanisms of rabies transmission from animal to person are biting and scratches, however, other ways, such as licking are also possible (3).
World Health Organization estimates that 40,000 to 70,000 people die each year from rabies in endemic countries (4). The annual incidence of animal bites has increased in recent years. The incidence rate of animal bites in Iran and in East Azerbaijan province reported 177 and 240 case per 100,000 persons, respectively (5).
Rabies can be prevented after a bite, and while wound washing and disinfecting wounds can prevent up to third of likely rabies infections and the administration of post-exposure prophylaxis (PEP) can also prevent death from rabies entirely (6). Timely PEP has not performed in some rabies endemic countries. Distance from the PEP center, animal type, severity of injuries, sex and residence location have all been recorded significant reasons for delayed PEP (7, 8). The majority of rabies deaths occur in people who have not had PEP, or who have received it in an insufficient or delayed manner (9).
Predictions shows that Iran's elder population will rise from 9.2% in 2015 to 23% in 2030 (10). Reflexes, skin thickness, subcutaneous adipose tissue, eyesight acuity, and system performance all decrease with age, making the older adults more susceptible to diseases and traumas than other age groups (11). A number of authors have reported analyses of trends in bites demonstrated about that bite injuries in elderly individuals account for about 10% of all bites (12, 13). In Iranian population, 37.2% of bite cases receive timely (< six hrs.) PEP services. Delayed (> six hrs.) PEP had been reported in 62.8% victims, which older adults contribute eight percent of delayed PEP (7).
The older people has a higher risk of injury severity, hospitalization, and postponed PEP than other age groups (12). Some cross-sectional studies suggest an association between financial, physical and psychological problems and delayed health services using older adults (14-16). According to Addai and Nuertey (2020), the declining trend of animal bites in in older adults is possibly due to shifting health-seeking behaviors and tend to ignore minor health threats (9).
Whilst some research has been carried out on the epidemiology of animal bite in Iran (5), no studies have been found which investigate predictors of delayed PEP in elder population. Our study aimed to investigate the pattern of delayed PEP in animal-bites victims and to identify its contributing factors in older persons of Tabriz city, Iran.
Methods
Study design
In this cross-sectional study, the census method used to obtain data from health records of 322 older adults who were referred to Tabriz's Rabies Treatment Center (Tabriz's RTC).
Setting and participants
Tabriz metropolitan in East Azerbaijan – Iran, covers an area of 11800 km2 with a population of about 1.5 million, according to the latest census data (17). The participants were aged 60 and over, and they were from both rural and urban backgrounds. The participants in this study were elderly persons who had been bitten by an animal and had referred to Tabriz's RTC to get PEP. Tabriz's RTC provides rabies prevention cares for Tabriz city and countryside villages including 44 health home, 15 rural health center.
Data collection
The inclusion criteria were older person animal bite cases that were reported during the dates 21st March 2013 and 20st March 2018. Incomplete records were excluded.
Demographical, epidemiological, and clinical characteristics were collected and analyzed. Demographic characteristics included age, sex, and the occupation status. Epidemiological characteristics comprised residency place [city/village], bitten animal status [domestic / wild], injury time [hour, day, month, season, year], and previous bite history. Clinical characteristics consist of the exact site of the bite/exposure, a number of bite sites, extent and depth of injury, location of injury [lower limbs, abdomen and upper limbs and head] variables. Also, PEP (vaccine/ rabies immunoglobulin [RIG]) data were included.
Ethical consideration
The Protocol of study was approved by the Regional Ethics Committee at Tabriz University of Medical Sciences (Ethical code: IR.TBZMED.REC.1397.1096). The information was collected in a confidential and without identification of participants.
Statistical analysis
Mean ± standard deviation (SD) was used for quantitative data and frequency and percent were presented for qualitative characteristics.
At first, the variables of interest were analyzed to find significant ones in univariate tests. To explore the probable correlations between the qualitative variables, Chi-square test was applied. In situations of low sample size, Fisher's exact test was applied in univariate tests. Then significant variables were entered into the decision tree model.
The decision tree model is a powerful and common graphical method for classification and prediction (18). It has been used in predicting delayed PEP for animal bite victims in Iran (8).
The decision tree is usually composed of several nodes known as input and output nodes. The rules created in the decision tree are expressed as "if" and "then”. Predictive tree modeling and regression is a nonparametric algorithmic method that is able to predict quantitative variables (regression tree) or classified variables (classification tree) based on a set of quantitative or qualitative predictor variables. With the intention of conducting a decision tree model, determining significant variables, the classification, and regression trees (CART) algorithm and Gini index were used (13).
In all statistical tests, the P-value less than 0.05 was considered as significant. Statistical analyses were done using SPSS V.21 (SPSS Inc, Chicago, IL, USA).
Results
From 21th March 2013 to 20th March 2018, 322 elder's bite victims referred to getting PEP in Tabriz's RTC were investigated.
The age of participants ranged from 60 to 90 years (67.62 ± 7.1 years). A total of 93% were from rural areas. In terms of the event site, 6.86% had happened in urban areas. Of the 322 participants, 20 (six percent) had a history of previous animal bite exposure. From the aspect of getting PEP, 29.2% received the 5-dose intramuscular vaccination schedule, 66.5% received 3-dose vaccine and 4.3% received < 3-dose vaccine. Of all victims, 14.6% (received RIG alongside vaccine. Ninety-six percent of participants had received the PEP program, albeit with some delays. Most of those affected people were self-employed and housewives. In terms of the time of injuries, most events occurred between 6-12 AM.
The prevalence of a delayed PEP was 31.7 % of older adult patients. The delayed PEP was more observed in females than males (34.3% vs. 31.0%), (p =0.06). The results of univariate analysis are revealed in Table 1. The prevalence of delayed PEP was significantly higher in urban older adults than rural (p =0.02). There was a significant relationship between the biting animal species and the time for seeking PEP. Older people bitten by dogs, delay prevalence were 23.8%, elders attacked by other animals, prevalence of delay was 39.9% (p=0.002). There was a relationship between the animal ownership status and delay time of PEP, with 42 percent delayed following stray animal bites compared to 24.6 percent in others. The Fisher's Exact Test between animal status and delayed PEP revealed that the frequency of delay in injuries in which the attacking animal escaped was significantly higher than in case of killed and living animals (p=0.006).
Delay in superficial injuries was higher than deep injuries, 33.7% and 19.6%, respectively (p = 0.056). Based on the findings of Table 1, residency-event, type of animal, animal ownership status, and animal status variables which had a significant effect on the delayed time of PEP were placed on the decision tree modeling. The Gini index, as an impure function of CART algorithm, showed that the most important variables for predicting the delayed PEP were being stray animal, the animal’s status and animal species, respectively. (Figure 1)
According to figure 1, three following rules can be understood:
A. If” the animal is stray and escaped” then the probability of delayed PEP is 46.2%.
B. If “The animal is NOT stray” and “The animal is NOT a dog” then the probability of delayed PEP is 39.7%.
C. If “The animal is being stray” and “The animal is alive”, then the probability of delayed PEP is 35.3%.
Discussion
It is important to initiate PEP immediately. In fact, this is one of the first studies in Iran to examine the factors linked to delayed PEP in older people. In various studies, elder population were at least 10% of all animal bite victims (7, 19). Older adults who do not receive timely and complete PEP, experience high rates of rabies and premature death (20). This study identified, animal ownership status, animal status and animal species as contributing factors on the delayed PEP.
In the present study, delayed PEP was observed in 31.7% of participants which is lower than the delay time proportion in Tuyserkan, Iran (68.2%) (7). This different delay time maybe due to the difference between mean age and health behavior among studies. It has been shown that there is an association between timely PEP and age (21). Older individuals are more likely than youths to follow health recommendations, because they have a better understanding of health-threats and use healthcare services (22-24). Teenagers perception of the risk of participating in health-treating activities is lower than that of older adults (25). Also, in older persons, vaccine adherence rises with the number of medical visits per year (24).
Other studies of delayed PEP in different age groups, including Khaf county, Iran reported 14.4% in women and 5.2% in men (26). Also in a study from Ilam, Iran delayed PEP(> 13 h) had been reported 18.1 percent (19), which were different from our study estimation. A possible explanation for this might be that there was association between distance from RTC and place of residence and timely PEP. These finding reflect those of Khazaei et al. who also found that a majority of delayed PEP cases have more than thirty kilometers distance from RTC (7).
Table 1. Univariate analysis of the relationship between demographic variables, animal status, injured organ, and delay of more than 24 hours after animal bite for post-exposure prophylaxis, vaccination in older adults in Tabriz
* Cat, Horse, Donkey, wolf, Cow, Sheep, Camel, Fox, Jackal, Pig and Goat
**Fisher’s Exact Test
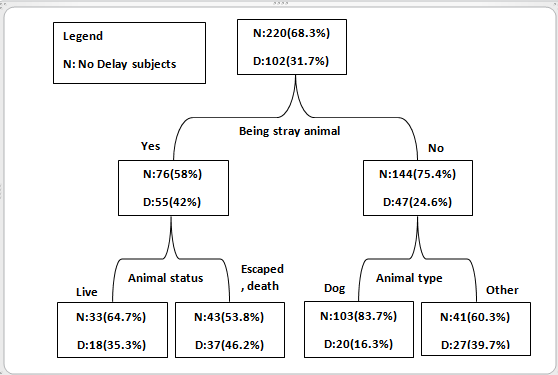
Figure1. Final decision tree model for predicting delayed PEP using classification and regression tree algorithm
According to the decision tree technique, cases bitten by cats, foxes, wolves, jackals, horses, donkeys, cows, camels, pigs, sheep and goats have a more delayed PEP than dog victims, this also accords with Hamta et al.(27) study in the center of Iran, also accords with our earlier observations, which revealed that individuals bitten by cats had a higher rate of PEP delay (28). In a study from Hamadan, Iran, cat bite victims had the most significant delayed PEP (29).
Higher delay time in PEP for animals other than dogs is due to the focus of the Iranian Ministry of Health's programs on dog bite, like vaccination of dogs and restricting their movement and neglect to other animals (30). Another possible explanation for this delay is the lack of public awareness about transmission of rabies from animals other than dog and cat.
In this study delay time was found more prevalent superficial injury than deep injuries. Deep injuries in other studies in Iran were between 15 and 28% (7, 31, 32). In a study in China, 61.3% of cases had a deep injury type (33). In the most severe injury cases timely and urgency health care seeking behavior is common. Only 14.6% of the subjects of the exposed victims, had a deep injury which was in agreement with the findings of Khazaei et al. (7) and Rafiei et al. (34) studies with 15.8% and 20.9% deep injury types respectively. The experiences of serious injuries can force them to obtain a complete care to optimize anti-rabies prevention. In contrast delayed time of superficial can be due to the low-risk perception, reduced sense of pain and lack of self-care. In the present study, lower frequency of deep injuries could be due to the high percentage of bites of animals like cats, foxes, wolves, jackals, horses, donkeys, cows, camels, pigs, sheep and goats.
In our study the prevalence of delay among urban older adults was significantly higher than rural older adults, while in the studies of Hamadan-Iran (29), Aq Qala, Iran (31), Tanzania (34) and India (35), rural bites injuries have been delayed in receiving PEP due to the long distance to the rabies prevention center and the high cost of transportation. One of the probable explanations behind this condition may be the effects of a “training day” program in the countryside. Training day is a one- or two-day program, according to population size and priority of educational topics in health homes in the Iranian villages. Health education can lead to behavior change and performance improvement.
About three quarters of events were taking place in the urban residency. The Tabriz's urbanization, slum marginalized population has rapidly grown in recent decades. Also, pet keeping in cities has increased in recent years, probably leading to increased levels of exposure to animals.
Also, in the present study, delayed PEP was significantly in stray animal victims more than in domestic animals. Which is in line with the Khazei findings (7). People with pets appear to be more aware of the common zoonosis disease than other populations, especially about rabies (36-38). Based on the decision tree results, delay in injuries caused by escaping animals was significantly greater than live or killed animals. The largest percentage of escaped animals were cats, foxes, wolves, jackals, horses, donkeys, cows, camels, pigs, sheep and goats. The bites of these animals appear to be considered low risk and therefore the older adults are less likely to seek acute care in such injuries.
Conclusion
About one third of the subjects showed the delayed PEP after animal bite. The most important factors affecting delay time were animal species, animal ownership status and older adults’ residence. It seemed that injuries of cats, foxes, wolves and other animals in comparison to dogs are considered to be less risky amongst participants that necessitate serious attention to be highlighted in various health educational and promotional programs. Also, it seems that the PEP follow-up process of the urban older adults is less than rural Health-Home follow up care. Therefore, active follow-up of urban elder population needs more attention in the target population.
Study limitations
There were a few limitations in this study. The assessment of a rabies monitoring system necessitates the use of reliable data sources. We used information from Tabriz's RTC's databases. Information bias is likely because the quality and accuracy of the data is mostly determined by the quality and accuracy of the recorded data. However, the delayed PEP may be underestimated in the present study, because some of the exposed older adults’ victims refuse to refer to health centers for PEP vaccinations, particularly for minor injury events. This is the study's primary problem, which could lead to selection bias.
Acknowledgement
The authors would like to thank the rabies center staff of the Tabriz Health Network for collaborating on data collection.
Conflict of interest
All of the authors state that they have no conflict of interest.
Authors' contributions
All authors read the final draft of the manuscript, provided the necessary revisions, and accepted the responsibility its contents.
References
Full-Text: (887 Views)
Predictors of Delay in Seeking Post-Exposure Prophylaxis in Older Adults with Animal Bite Injuries: A Population-Based Study
Hassan Soleimanpour 1, Mehdi Abbasian 2,3, Ehsan Sarbazi 4,5,6*, Seyed Pouya Paknezhad 1, Hadi Jalilvand 7, Nazanin Masoudi 7, Hosein Azizi 8, Zahra Khalili 9
Hassan Soleimanpour 1, Mehdi Abbasian 2,3, Ehsan Sarbazi 4,5,6*, Seyed Pouya Paknezhad 1, Hadi Jalilvand 7, Nazanin Masoudi 7, Hosein Azizi 8, Zahra Khalili 9
- Emergency Medicine Research Team, Tabriz University of Medical Sciences, Tabriz, Iran
- Department of Geriatric Health, Faculty of Health Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
- Research Center for Integrative Medicine in Aging, Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
- Road Traffic Injury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
- Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
- Tabriz Health Services Management Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
- Department of Statistics and Epidemiology, Faculty of Health Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
- Research Center of Psychiatry and Behavioral Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
- Department of Nursing and Midwifery, School of Nursing and Midwifery, Ardabil University of Medical Sciences, Ardabil, Iran
Article history
Received 5 Sep 2021
Accepted 31 Oct 2021
A B S T R A C T
Introduction: Animal bites are of the major health threats. Delayed post-exposure prophylaxis (PEP), especially in frail older people, may lead to mortal risks in this age group. The aim of this study was to investigate the pattern of delayed PEP in animal-bites injuries and to identify its contributing factors in older people of Tabriz city, Iran.
Methods: In this cross-sectional study, the census method was used to obtain data from health records of older adults who were referred to Tabriz's Rabies Treatment Center between March 2013 and March 2018. The delay was defined as starting PEP longer than 24 hours after a suspected rabies virus exposure. The relations between delayed PEP and each of the predictors were investigated using the chi-square test in univariate analysis. The decision tree model was applied to predict the delay time of PEP.
Results: A total of 322 older people with a mean age of 67.62 ± 7.18 were studied. In all, 31.7 % of the older persons victims who were bitten by an animal had a delayed PEP. Urban victims (34.1%) compared to rural (16.3 %), stray animal victims (42.0 %) compared to an owned animal-bite victim 24.6 %, all other animal bite-related victims (39.9 %) compared to dog-bite injuries (23.8%) experienced a higher frequency of delayed PEP. The decision tree revealed that animal ownership status, animal status, and animal species were the most important factors for predicting delayed PEP (p < 0.001).
Conclusion: The possibility of delayed PEP in older adults bites victims, increased if the animal was ownerless and escaped. A reasonable approach to tackle this issue might be to conduct larger population studies in the future.
Keywords: Post-Exposure Prophylaxis, Decision Tree, Bite Injury, Delay of Vaccine
Received 5 Sep 2021
Accepted 31 Oct 2021
A B S T R A C T
Introduction: Animal bites are of the major health threats. Delayed post-exposure prophylaxis (PEP), especially in frail older people, may lead to mortal risks in this age group. The aim of this study was to investigate the pattern of delayed PEP in animal-bites injuries and to identify its contributing factors in older people of Tabriz city, Iran.
Methods: In this cross-sectional study, the census method was used to obtain data from health records of older adults who were referred to Tabriz's Rabies Treatment Center between March 2013 and March 2018. The delay was defined as starting PEP longer than 24 hours after a suspected rabies virus exposure. The relations between delayed PEP and each of the predictors were investigated using the chi-square test in univariate analysis. The decision tree model was applied to predict the delay time of PEP.
Results: A total of 322 older people with a mean age of 67.62 ± 7.18 were studied. In all, 31.7 % of the older persons victims who were bitten by an animal had a delayed PEP. Urban victims (34.1%) compared to rural (16.3 %), stray animal victims (42.0 %) compared to an owned animal-bite victim 24.6 %, all other animal bite-related victims (39.9 %) compared to dog-bite injuries (23.8%) experienced a higher frequency of delayed PEP. The decision tree revealed that animal ownership status, animal status, and animal species were the most important factors for predicting delayed PEP (p < 0.001).
Conclusion: The possibility of delayed PEP in older adults bites victims, increased if the animal was ownerless and escaped. A reasonable approach to tackle this issue might be to conduct larger population studies in the future.
Keywords: Post-Exposure Prophylaxis, Decision Tree, Bite Injury, Delay of Vaccine
Copyright © 2021 Elderly Health Journal. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cite.
Introduction
Animal bites is one of the major health threats specially in rabies endemic areas, because in every bite is potentially a suspected exposure (1). Rabies is a viral infection that affects mammals' central nervous systems and is fatal once symptoms appear (2). The two main mechanisms of rabies transmission from animal to person are biting and scratches, however, other ways, such as licking are also possible (3).
World Health Organization estimates that 40,000 to 70,000 people die each year from rabies in endemic countries (4). The annual incidence of animal bites has increased in recent years. The incidence rate of animal bites in Iran and in East Azerbaijan province reported 177 and 240 case per 100,000 persons, respectively (5).
Rabies can be prevented after a bite, and while wound washing and disinfecting wounds can prevent up to third of likely rabies infections and the administration of post-exposure prophylaxis (PEP) can also prevent death from rabies entirely (6). Timely PEP has not performed in some rabies endemic countries. Distance from the PEP center, animal type, severity of injuries, sex and residence location have all been recorded significant reasons for delayed PEP (7, 8). The majority of rabies deaths occur in people who have not had PEP, or who have received it in an insufficient or delayed manner (9).
Predictions shows that Iran's elder population will rise from 9.2% in 2015 to 23% in 2030 (10). Reflexes, skin thickness, subcutaneous adipose tissue, eyesight acuity, and system performance all decrease with age, making the older adults more susceptible to diseases and traumas than other age groups (11). A number of authors have reported analyses of trends in bites demonstrated about that bite injuries in elderly individuals account for about 10% of all bites (12, 13). In Iranian population, 37.2% of bite cases receive timely (< six hrs.) PEP services. Delayed (> six hrs.) PEP had been reported in 62.8% victims, which older adults contribute eight percent of delayed PEP (7).
The older people has a higher risk of injury severity, hospitalization, and postponed PEP than other age groups (12). Some cross-sectional studies suggest an association between financial, physical and psychological problems and delayed health services using older adults (14-16). According to Addai and Nuertey (2020), the declining trend of animal bites in in older adults is possibly due to shifting health-seeking behaviors and tend to ignore minor health threats (9).
Whilst some research has been carried out on the epidemiology of animal bite in Iran (5), no studies have been found which investigate predictors of delayed PEP in elder population. Our study aimed to investigate the pattern of delayed PEP in animal-bites victims and to identify its contributing factors in older persons of Tabriz city, Iran.
Methods
Study design
In this cross-sectional study, the census method used to obtain data from health records of 322 older adults who were referred to Tabriz's Rabies Treatment Center (Tabriz's RTC).
Setting and participants
Tabriz metropolitan in East Azerbaijan – Iran, covers an area of 11800 km2 with a population of about 1.5 million, according to the latest census data (17). The participants were aged 60 and over, and they were from both rural and urban backgrounds. The participants in this study were elderly persons who had been bitten by an animal and had referred to Tabriz's RTC to get PEP. Tabriz's RTC provides rabies prevention cares for Tabriz city and countryside villages including 44 health home, 15 rural health center.
Data collection
The inclusion criteria were older person animal bite cases that were reported during the dates 21st March 2013 and 20st March 2018. Incomplete records were excluded.
Demographical, epidemiological, and clinical characteristics were collected and analyzed. Demographic characteristics included age, sex, and the occupation status. Epidemiological characteristics comprised residency place [city/village], bitten animal status [domestic / wild], injury time [hour, day, month, season, year], and previous bite history. Clinical characteristics consist of the exact site of the bite/exposure, a number of bite sites, extent and depth of injury, location of injury [lower limbs, abdomen and upper limbs and head] variables. Also, PEP (vaccine/ rabies immunoglobulin [RIG]) data were included.
Ethical consideration
The Protocol of study was approved by the Regional Ethics Committee at Tabriz University of Medical Sciences (Ethical code: IR.TBZMED.REC.1397.1096). The information was collected in a confidential and without identification of participants.
Statistical analysis
Mean ± standard deviation (SD) was used for quantitative data and frequency and percent were presented for qualitative characteristics.
At first, the variables of interest were analyzed to find significant ones in univariate tests. To explore the probable correlations between the qualitative variables, Chi-square test was applied. In situations of low sample size, Fisher's exact test was applied in univariate tests. Then significant variables were entered into the decision tree model.
The decision tree model is a powerful and common graphical method for classification and prediction (18). It has been used in predicting delayed PEP for animal bite victims in Iran (8).
The decision tree is usually composed of several nodes known as input and output nodes. The rules created in the decision tree are expressed as "if" and "then”. Predictive tree modeling and regression is a nonparametric algorithmic method that is able to predict quantitative variables (regression tree) or classified variables (classification tree) based on a set of quantitative or qualitative predictor variables. With the intention of conducting a decision tree model, determining significant variables, the classification, and regression trees (CART) algorithm and Gini index were used (13).
In all statistical tests, the P-value less than 0.05 was considered as significant. Statistical analyses were done using SPSS V.21 (SPSS Inc, Chicago, IL, USA).
Results
From 21th March 2013 to 20th March 2018, 322 elder's bite victims referred to getting PEP in Tabriz's RTC were investigated.
The age of participants ranged from 60 to 90 years (67.62 ± 7.1 years). A total of 93% were from rural areas. In terms of the event site, 6.86% had happened in urban areas. Of the 322 participants, 20 (six percent) had a history of previous animal bite exposure. From the aspect of getting PEP, 29.2% received the 5-dose intramuscular vaccination schedule, 66.5% received 3-dose vaccine and 4.3% received < 3-dose vaccine. Of all victims, 14.6% (received RIG alongside vaccine. Ninety-six percent of participants had received the PEP program, albeit with some delays. Most of those affected people were self-employed and housewives. In terms of the time of injuries, most events occurred between 6-12 AM.
The prevalence of a delayed PEP was 31.7 % of older adult patients. The delayed PEP was more observed in females than males (34.3% vs. 31.0%), (p =0.06). The results of univariate analysis are revealed in Table 1. The prevalence of delayed PEP was significantly higher in urban older adults than rural (p =0.02). There was a significant relationship between the biting animal species and the time for seeking PEP. Older people bitten by dogs, delay prevalence were 23.8%, elders attacked by other animals, prevalence of delay was 39.9% (p=0.002). There was a relationship between the animal ownership status and delay time of PEP, with 42 percent delayed following stray animal bites compared to 24.6 percent in others. The Fisher's Exact Test between animal status and delayed PEP revealed that the frequency of delay in injuries in which the attacking animal escaped was significantly higher than in case of killed and living animals (p=0.006).
Delay in superficial injuries was higher than deep injuries, 33.7% and 19.6%, respectively (p = 0.056). Based on the findings of Table 1, residency-event, type of animal, animal ownership status, and animal status variables which had a significant effect on the delayed time of PEP were placed on the decision tree modeling. The Gini index, as an impure function of CART algorithm, showed that the most important variables for predicting the delayed PEP were being stray animal, the animal’s status and animal species, respectively. (Figure 1)
According to figure 1, three following rules can be understood:
A. If” the animal is stray and escaped” then the probability of delayed PEP is 46.2%.
B. If “The animal is NOT stray” and “The animal is NOT a dog” then the probability of delayed PEP is 39.7%.
C. If “The animal is being stray” and “The animal is alive”, then the probability of delayed PEP is 35.3%.
Discussion
It is important to initiate PEP immediately. In fact, this is one of the first studies in Iran to examine the factors linked to delayed PEP in older people. In various studies, elder population were at least 10% of all animal bite victims (7, 19). Older adults who do not receive timely and complete PEP, experience high rates of rabies and premature death (20). This study identified, animal ownership status, animal status and animal species as contributing factors on the delayed PEP.
In the present study, delayed PEP was observed in 31.7% of participants which is lower than the delay time proportion in Tuyserkan, Iran (68.2%) (7). This different delay time maybe due to the difference between mean age and health behavior among studies. It has been shown that there is an association between timely PEP and age (21). Older individuals are more likely than youths to follow health recommendations, because they have a better understanding of health-threats and use healthcare services (22-24). Teenagers perception of the risk of participating in health-treating activities is lower than that of older adults (25). Also, in older persons, vaccine adherence rises with the number of medical visits per year (24).
Other studies of delayed PEP in different age groups, including Khaf county, Iran reported 14.4% in women and 5.2% in men (26). Also in a study from Ilam, Iran delayed PEP(> 13 h) had been reported 18.1 percent (19), which were different from our study estimation. A possible explanation for this might be that there was association between distance from RTC and place of residence and timely PEP. These finding reflect those of Khazaei et al. who also found that a majority of delayed PEP cases have more than thirty kilometers distance from RTC (7).
Table 1. Univariate analysis of the relationship between demographic variables, animal status, injured organ, and delay of more than 24 hours after animal bite for post-exposure prophylaxis, vaccination in older adults in Tabriz
| p-value | Delay | Total | Subcategories | Factors affecting the delay | |
| Yes, n (%) | No, n (%) | ||||
| 0.60 | 79(31.0) | 176(69.0) | 225 | Male | Sex |
| 23 (34.3) | 44 (65.7) | 67 | Female | ||
| 0.166 | 8 (42.1) | 11 (57.9) | 19 | Labor | Occupational status |
| 16 (33.3) | 32 (66.7) | 48 | Retired | ||
| 19 (30.2) | 44 (69.8) | 63 | Housekeeper | ||
| 6 (15.4) | 33(84.6) | 39 | Agriculture and driver | ||
| 53 (34.6) | 100 (65.4) | 153 | Self-employed | ||
| 0.604 | 80 (31.0) | 178 (69.0) | 258 | 0-12AM | Time of event |
| 22 (34.4) | 42 (65.6) | 64 | 13-24PM | ||
| 0.02 | 95 (34.1) | 184 (65.9) | 279 | Urban | Residency-event |
| 7 (16.3) | 36 (83.7) | 43 | Rural | ||
| 0.002 | 39 (23.8) | 125 (76.2) | 164 | Dog | Type of animal |
| 63 (39.9) | 95 (60.1) | 158 | Other* | ||
| 0.001 | 55 (42.0) | 76 (58.0) | 131 | Yes | Being stray |
| 47 (24.6) | 144 (75.4) | 191 | No | ||
| 0.413 | 79 (32.9) | 161 (67.1) | 240 | Upper limb of the human body | Injured organ |
| 23 (28.0) | 59 (72.0) | 82 | Lower limb of the human body | ||
| 0.056 | 93 (33.7) | 183 (66.3) | 276 | Superficial | Injury type |
| 9 (19.6) | 37 (80.4) | 46 | Deep | ||
| 0.118 | 45 (26.6) | 124 (73.4) | 169 | Spring | Season |
| 38 (40.9) | 55 (59.1) | 93 | Summer | ||
| 12 (34.3) | 23 (65.7) | 35 | Fall | ||
| 7 (28.0) | 18 (72.0) | 25 | Winter | ||
| 0.733 | 84 (30.9) | 188 (69.1) | 272 | 60-75 | Age** |
| 16 (37.2) | 27 (62.8) | 43 | 75-85 | ||
| 2 (28.6) | 5 (71.4) | 7 | > 85 | ||
| 0.006 | 63 (26.9) | 171 (73.1) | 234 | Live | Status of animal** |
| 37 (45.7) | 44 (54.3) | 81 | Escaped | ||
| 2 (28.6) | 5 (71.5) | 7 | Kill | ||
* Cat, Horse, Donkey, wolf, Cow, Sheep, Camel, Fox, Jackal, Pig and Goat
**Fisher’s Exact Test
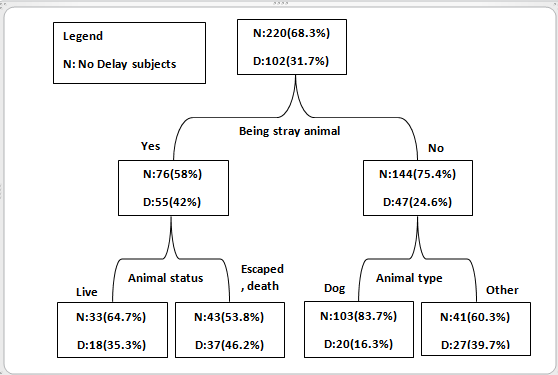
Figure1. Final decision tree model for predicting delayed PEP using classification and regression tree algorithm
According to the decision tree technique, cases bitten by cats, foxes, wolves, jackals, horses, donkeys, cows, camels, pigs, sheep and goats have a more delayed PEP than dog victims, this also accords with Hamta et al.(27) study in the center of Iran, also accords with our earlier observations, which revealed that individuals bitten by cats had a higher rate of PEP delay (28). In a study from Hamadan, Iran, cat bite victims had the most significant delayed PEP (29).
Higher delay time in PEP for animals other than dogs is due to the focus of the Iranian Ministry of Health's programs on dog bite, like vaccination of dogs and restricting their movement and neglect to other animals (30). Another possible explanation for this delay is the lack of public awareness about transmission of rabies from animals other than dog and cat.
In this study delay time was found more prevalent superficial injury than deep injuries. Deep injuries in other studies in Iran were between 15 and 28% (7, 31, 32). In a study in China, 61.3% of cases had a deep injury type (33). In the most severe injury cases timely and urgency health care seeking behavior is common. Only 14.6% of the subjects of the exposed victims, had a deep injury which was in agreement with the findings of Khazaei et al. (7) and Rafiei et al. (34) studies with 15.8% and 20.9% deep injury types respectively. The experiences of serious injuries can force them to obtain a complete care to optimize anti-rabies prevention. In contrast delayed time of superficial can be due to the low-risk perception, reduced sense of pain and lack of self-care. In the present study, lower frequency of deep injuries could be due to the high percentage of bites of animals like cats, foxes, wolves, jackals, horses, donkeys, cows, camels, pigs, sheep and goats.
In our study the prevalence of delay among urban older adults was significantly higher than rural older adults, while in the studies of Hamadan-Iran (29), Aq Qala, Iran (31), Tanzania (34) and India (35), rural bites injuries have been delayed in receiving PEP due to the long distance to the rabies prevention center and the high cost of transportation. One of the probable explanations behind this condition may be the effects of a “training day” program in the countryside. Training day is a one- or two-day program, according to population size and priority of educational topics in health homes in the Iranian villages. Health education can lead to behavior change and performance improvement.
About three quarters of events were taking place in the urban residency. The Tabriz's urbanization, slum marginalized population has rapidly grown in recent decades. Also, pet keeping in cities has increased in recent years, probably leading to increased levels of exposure to animals.
Also, in the present study, delayed PEP was significantly in stray animal victims more than in domestic animals. Which is in line with the Khazei findings (7). People with pets appear to be more aware of the common zoonosis disease than other populations, especially about rabies (36-38). Based on the decision tree results, delay in injuries caused by escaping animals was significantly greater than live or killed animals. The largest percentage of escaped animals were cats, foxes, wolves, jackals, horses, donkeys, cows, camels, pigs, sheep and goats. The bites of these animals appear to be considered low risk and therefore the older adults are less likely to seek acute care in such injuries.
Conclusion
About one third of the subjects showed the delayed PEP after animal bite. The most important factors affecting delay time were animal species, animal ownership status and older adults’ residence. It seemed that injuries of cats, foxes, wolves and other animals in comparison to dogs are considered to be less risky amongst participants that necessitate serious attention to be highlighted in various health educational and promotional programs. Also, it seems that the PEP follow-up process of the urban older adults is less than rural Health-Home follow up care. Therefore, active follow-up of urban elder population needs more attention in the target population.
Study limitations
There were a few limitations in this study. The assessment of a rabies monitoring system necessitates the use of reliable data sources. We used information from Tabriz's RTC's databases. Information bias is likely because the quality and accuracy of the data is mostly determined by the quality and accuracy of the recorded data. However, the delayed PEP may be underestimated in the present study, because some of the exposed older adults’ victims refuse to refer to health centers for PEP vaccinations, particularly for minor injury events. This is the study's primary problem, which could lead to selection bias.
Acknowledgement
The authors would like to thank the rabies center staff of the Tabriz Health Network for collaborating on data collection.
Conflict of interest
All of the authors state that they have no conflict of interest.
Authors' contributions
All authors read the final draft of the manuscript, provided the necessary revisions, and accepted the responsibility its contents.
References
- World Health Organization. WHO expert consultation on rabies: third report [Internet]. World Health Organization; 2018 [cited 2021 May 12]. Available from: https://apps.who.int/iris/handle/10665/272364
- Ripani A, Mérot J, Bouguedour R, Zrelli M. Review of rabies situation and control in the North African region with a focus on Tunisia. Revue Scientifique et Technique (International Office of Epizootics). 2017; 36(3): 1-16.
- Singh R, Singh KP, Cherian S, Saminathan M, Kapoor S, Manjunatha Reddy G, et al. Rabies–epidemiology, pathogenesis, public health concerns and advances in diagnosis and control: a comprehensive review. The Veterinary Quarterly. 2017; 37(1): 212-51.
- World Health Organization. Rabies vaccines: WHO position paper, April 2018–Recommendations. Vaccine. 2018; 36(37): 5500-3.
- Abedi M, Doosti-Irani A, Jahanbakhsh F, Sahebkar A. Epidemiology of animal bite in Iran during a 20-year period (1993–2013): a meta-analysis. Tropical Medicine and Health. 2019; 47(1): 1-13.
- Kisaka S, Makumbi FE, Majalija S, Bangirana A, Thumbi S. Epidemiology and preclinical management of dog bites among humans in Wakiso and Kampala districts, Uganda: implications for prevention of dog bites and rabies. PloS One. 2020; 15(9): 1-21.
- Khazaei S, Rezaeian S, Soheylizad M, Gholamaliee B. Factors associated with delay in post-exposure prophylaxis in bitten people. Medical Journal of the Islamic Republic of Iran. 2014; 28(158): 1-7.
- Sarbazi E, Sarbazi M, Ghaffari-Fam S, Babazadeh T, Heidari S, Aghakarimi K, et al. Factors related to delay in initiating post-exposure prophylaxis for rabies prevention among animal bite victims: a cross-sectional study in Northwest of Iran. Bulletin of Emergency & Trauma. 2020; 8(4): 236-42.
- Addai JA, Nuertey BD. Pattern of animal bites and delays in initiating rabies postexposure prophylaxis among clients receiving care in korle-bu teaching hospital. Journal of Tropical Medicine. 2020; 2020(4): 1-6.
- Mirzaie M, Darabi S. Population aging in Iran and rising health care costs. Salmand: Iranian Journal of Ageing. 2017; 12 (2): 156-69
- Fillit HM, Rockwood K, Young JB. Brocklehurst's textbook of geriatric medicine and gerontology. 8th Edition. Elsevier Health Sciences; 2016.
- Loder RT. The demographics of dog bites in the United States. Heliyon. 2019; 5(3): e01360.
- Suraweera W, Morris SK, Kumar R, Warrell DA, Warrell MJ, Jha P, et al. Deaths from symptomatically identifiable furious rabies in India: a nationally representative mortality survey. PLoS Neglected Tropical Diseases. 2012; 6(10): 1-9.
- Wani RT, Chowdri IN, Dar H. Factors influencing delay in initiating post-exposure prophylaxis for rabies prevention among animal bite victims: a cross sectional study. Journal of Family Medicine and Primary Care. 2020; 9(9): 4751-5.
- Joseph J, Sangeetha N, Khan AM, Rajoura O. Determinants of delay in initiating post-exposure prophylaxis for rabies prevention among animal bite cases: hospital based study. Vaccine. 2013; 32(1): 74-7.
- Esmaeilzadeh F, Rajabi A, Vahedi S, Shamsadiny M, Ghojogh MG, Hatam N. Epidemiology of animal bites and factors associated with delays in initiating post-exposure prophylaxis for rabies prevention among animal bite cases: A population-based study. Journal of Preventive Medicine and Public Health. 2017; 50(3): 210-6.
- Azarafza M, Ghazifard A. Urban geology of Tabriz city: environmental and geological constraints. Advances in Environmental Research. 2016; 5(2): 95-108.
- Han J, Pei J, Kamber M. Data mining: concepts and techniques. Third Edition. Elsevier; 2011.
- Kassiri H, Lotfi M, Ebrahimi A. Epidemiological and demographic study of acute animal biting in Abdanan County, Ilam Province, Western Iran. Journal of Acute Disease. 2017; 6(6): 272-7.
- Romero-Sengson RF. Factors affecting compliance to rabies post-exposure prophylaxis among pediatric patients seen at the research institute for tropical medicine. Pediatric Infectious Disease Society of the Philippines Journal. 2013; 14(2): 56-62.
- Riahi S, Latifi A, Bakhtiyari M, Yavari P, Khezeli M, Hatami H. Epidemiologic survey of animal bites and causes of delay in getting preventive treatment in Tabbas during 2005-2010. Tolooebehdasht. 2012; 11(1): 20-31.[Persian]
- Brandão MdPM, Martins L, Szewczyczak M, Talarska D, Philp I, Cardoso MF. Threats to health and well-being perceived by older people in Poland and Portugal. Acta Medica Portuguesa. 2018; 31(7-8): 409-15.
- Thumé E, Facchini LA, Wyshak G, Campbell P. The utilization of home care by the elderly in Brazil's primary health care system. American Journal of Public Health. 2011; 101(5): 868-74.
- Martínez-Baz I, Aguilar I, Morán J, Albéniz E, Aldaz P, Castilla J. Factors associated with continued adherence to influenza vaccination in the elderly. Preventive Medicine. 2012; 55(3): 246-50.
- Siren A, Kjær MR. How is the older road users’ perception of risk constructed?. Transportation Research Part F: Traffic Psychology and Behaviour. 2011; 14(3): 222-8.
- Samiee-Roudi K, Soltani M. Pattern of animal bites and factors associated with delay in post-exposure prophylaxis in bitten people. Chronic Diseases Journal. 2018; 6(4): 171-8.
- Hamta A, Saghafipour A, Hosseinalipour SA, Rezaei F. Forecasting delay times in post-exposure prophylaxis to human animal bite injuries in Central Iran: A decision tree analysis. Veterinary World. 2019; 12(7): 965-71.
- Gaffari-fam S, Sarbazi E, Moradpour H, Soleimanpour H, Azizi H, Heidari S. Epidemiological patterns, trends of animal bites and factors associated with delays in initiating post-exposure prophylaxis for rabies prevention in hurand, iran: a cross-sectional study. Journal of Clinical and Basic Research. 2021; 5(3): 1-8.
- Mohammadzadeh A, Mahmoodi P, Sharifi A, Moafi M, Erfani H, Siavashi M. A three-year epidemiological study of animal bites and rabies in Hamedan Province of Iran. Avicenna Journal Clinical Microbiology Infection. 2017; 4(2): 1-5.
- Bannazadeh Baghi H, Alinezhad F, Kuzmin I, Rupprecht CE. A perspective on rabies in the Middle East—Beyond Neglect. Veterinary Sciences. 2018; 5(3): 67.
- Tenzin T, Dhand NK, Ward MP. Human rabies post exposure prophylaxis in Bhutan, 2005–2008: trends and risk factors. Vaccine. 2011; 29(24): 4094-101.
- Sheikholeslami NZ, Rezaeian M, Salem Z. Epidemiology of animal bites in Rafsanjan, southeast of Islamic Republic of Iran, 2003-05. EMHJ-Eastern Mediterranean Health Journal. 2009; 15 (2): 455-7.
- Fang LX, Ping F, Hui BG, Yan YX. Socioeconomic status is a critical risk factor for human rabies post-exposure prophylaxis. Vaccine. 2010; 28(42): 6847-51.
- Rafiei N, Heshmati H, Taneh A. Animal bite and its contributors in aq-qala district, golestan province, Iran. Journal of Basic Research in Medical Sciences. 2014; 1(2): 36-42.
- Sambo M, Cleaveland S, Ferguson H, Lembo T, Simon C, Urassa H, et al. The burden of rabies in Tanzania and its impact on local communities. PLoS Neglected Tropical Diseases. 2013; 7(11): 1-9.
- Issah B, Ansah T, Alagma H. Awareness of zoonotic diseases among pet owners in wa municipality of ghana. UDS International Journal of Development. 2020; 7(2): 387-97.
- Hundal JS, Sodhi SS, Gupta A, Singh J, Chahal US. Awareness, knowledge, and risks of zoonotic diseases among livestock farmers in Punjab. Veterinary World. 2016; 9(2): 186-91.
- Özlü H, Atasever M, Atasever MA. Knowledge, attitude, and practices of cattle farmers regarding zoonotic diseases in Erzurum, Turkey. Austral Journal of Veterinary Sciences. 2020; 52(3): 79-85.
Type of Study: Research |
Subject:
Special
Received: 2021/09/5 | Accepted: 2021/10/31 | Published: 2021/12/19
Received: 2021/09/5 | Accepted: 2021/10/31 | Published: 2021/12/19
References
1. World Health Organization. WHO expert consultation on rabies: third report [Internet]. World Health Organization; 2018 [cited 2021 May 12]. Available from: https://apps.who.int/iris/handle/10665/272364
2. Ripani A, Mérot J, Bouguedour R, Zrelli M. Review of rabies situation and control in the North African region with a focus on Tunisia. Revue Scientifique et Technique (International Office of Epizootics). 2017; 36(3): 1-16.
3. Singh R, Singh KP, Cherian S, Saminathan M, Kapoor S, Manjunatha Reddy G, et al. Rabies–epidemiology, pathogenesis, public health concerns and advances in diagnosis and control: a comprehensive review. The Veterinary Quarterly. 2017; 37(1): 212-51.
4. World Health Organization. Rabies vaccines: WHO position paper, April 2018–Recommendations. Vaccine. 2018; 36(37): 5500-3.
5. Abedi M, Doosti-Irani A, Jahanbakhsh F, Sahebkar A. Epidemiology of animal bite in Iran during a 20-year period (1993–2013): a meta-analysis. Tropical Medicine and Health. 2019; 47(1): 1-13.
6. Kisaka S, Makumbi FE, Majalija S, Bangirana A, Thumbi S. Epidemiology and preclinical management of dog bites among humans in Wakiso and Kampala districts, Uganda: implications for prevention of dog bites and rabies. PloS One. 2020; 15(9): 1-21.
7. Khazaei S, Rezaeian S, Soheylizad M, Gholamaliee B. Factors associated with delay in post-exposure prophylaxis in bitten people. Medical Journal of the Islamic Republic of Iran. 2014; 28(158): 1-7.
8. Sarbazi E, Sarbazi M, Ghaffari-Fam S, Babazadeh T, Heidari S, Aghakarimi K, et al. Factors related to delay in initiating post-exposure prophylaxis for rabies prevention among animal bite victims: a cross-sectional study in Northwest of Iran. Bulletin of Emergency & Trauma. 2020; 8(4): 236-42.
9. Addai JA, Nuertey BD. Pattern of animal bites and delays in initiating rabies postexposure prophylaxis among clients receiving care in korle-bu teaching hospital. Journal of Tropical Medicine. 2020; 2020(4): 1-6.
10. Mirzaie M, Darabi S. Population aging in Iran and rising health care costs. Salmand: Iranian Journal of Ageing. 2017; 12 (2): 156-69.
11. Fillit HM, Rockwood K, Young JB. Brocklehurst's textbook of geriatric medicine and gerontology. 8th Edition. Elsevier Health Sciences; 2016.
12. Loder RT. The demographics of dog bites in the United States. Heliyon. 2019; 5(3): e01360.
13. Suraweera W, Morris SK, Kumar R, Warrell DA, Warrell MJ, Jha P, et al. Deaths from symptomatically identifiable furious rabies in India: a nationally representative mortality survey. PLoS Neglected Tropical Diseases. 2012; 6(10): 1-9.
14. Wani RT, Chowdri IN, Dar H. Factors influencing delay in initiating post-exposure prophylaxis for rabies prevention among animal bite victims: a cross sectional study. Journal of Family Medicine and Primary Care. 2020; 9(9): 4751-5.
15. Joseph J, Sangeetha N, Khan AM, Rajoura O. Determinants of delay in initiating post-exposure prophylaxis for rabies prevention among animal bite cases: hospital based study. Vaccine. 2013; 32(1): 74-7.
16. Esmaeilzadeh F, Rajabi A, Vahedi S, Shamsadiny M, Ghojogh MG, Hatam N. Epidemiology of animal bites and factors associated with delays in initiating post-exposure prophylaxis for rabies prevention among animal bite cases: A population-based study. Journal of Preventive Medicine and Public Health. 2017; 50(3): 210-6.
17. Azarafza M, Ghazifard A. Urban geology of Tabriz city: environmental and geological constraints. Advances in Environmental Research. 2016; 5(2): 95-108.
18. Han J, Pei J, Kamber M. Data mining: concepts and techniques. Third Edition. Elsevier; 2011.
19. Kassiri H, Lotfi M, Ebrahimi A. Epidemiological and demographic study of acute animal biting in Abdanan County, Ilam Province, Western Iran. Journal of Acute Disease. 2017; 6(6): 272-7.
20. Romero-Sengson RF. Factors affecting compliance to rabies post-exposure prophylaxis among pediatric patients seen at the research institute for tropical medicine. Pediatric Infectious Disease Society of the Philippines Journal. 2013; 14(2): 56-62.
21. Riahi S, Latifi A, Bakhtiyari M, Yavari P, Khezeli M, Hatami H. Epidemiologic survey of animal bites and causes of delay in getting preventive treatment in Tabbas during 2005-2010. Tolooebehdasht. 2012; 11(1): 20-31.[Persian]
22. Brandão MdPM, Martins L, Szewczyczak M, Talarska D, Philp I, Cardoso MF. Threats to health and well-being perceived by older people in Poland and Portugal. Acta Medica Portuguesa. 2018; 31(7-8): 409-15.
23. Thumé E, Facchini LA, Wyshak G, Campbell P. The utilization of home care by the elderly in Brazil's primary health care system. American Journal of Public Health. 2011; 101(5): 868-74.
24. Martínez-Baz I, Aguilar I, Morán J, Albéniz E, Aldaz P, Castilla J. Factors associated with continued adherence to influenza vaccination in the elderly. Preventive Medicine. 2012; 55(3): 246-50.
25. Siren A, Kjær MR. How is the older road users’ perception of risk constructed?. Transportation Research Part F: Traffic Psychology and Behaviour. 2011; 14(3): 222-8.
26. Samiee-Roudi K, Soltani M. Pattern of animal bites and factors associated with delay in post-exposure prophylaxis in bitten people. Chronic Diseases Journal. 2018; 6(4): 171-8.
27. Hamta A, Saghafipour A, Hosseinalipour SA, Rezaei F. Forecasting delay times in post-exposure prophylaxis to human animal bite injuries in Central Iran: A decision tree analysis. Veterinary World. 2019; 12(7): 965-71.
28. Gaffari-fam S, Sarbazi E, Moradpour H, Soleimanpour H, Azizi H, Heidari S. Epidemiological patterns, trends of animal bites and factors associated with delays in initiating post-exposure prophylaxis for rabies prevention in hurand, iran: a cross-sectional study. Journal of Clinical and Basic Research. 2021; 5(3): 1-8.
29. Mohammadzadeh A, Mahmoodi P, Sharifi A, Moafi M, Erfani H, Siavashi M. A three-year epidemiological study of animal bites and rabies in Hamedan Province of Iran. Avicenna Journal Clinical Microbiology Infection. 2017; 4(2): 1-5.
30. Bannazadeh Baghi H, Alinezhad F, Kuzmin I, Rupprecht CE. A perspective on rabies in the Middle East—Beyond Neglect. Veterinary Sciences. 2018; 5(3): 67.
31. Tenzin T, Dhand NK, Ward MP. Human rabies post exposure prophylaxis in Bhutan, 2005–2008: trends and risk factors. Vaccine. 2011; 29(24): 4094-101.
32. Sheikholeslami NZ, Rezaeian M, Salem Z. Epidemiology of animal bites in Rafsanjan, southeast of Islamic Republic of Iran, 2003-05. EMHJ-Eastern Mediterranean Health Journal. 2009; 15 (2): 455-7.
33. Fang LX, Ping F, Hui BG, Yan YX. Socioeconomic status is a critical risk factor for human rabies post-exposure prophylaxis. Vaccine. 2010; 28(42): 6847-51.
34. Rafiei N, Heshmati H, Taneh A. Animal bite and its contributors in aq-qala district, golestan province, Iran. Journal of Basic Research in Medical Sciences. 2014; 1(2): 36-42.
35. Sambo M, Cleaveland S, Ferguson H, Lembo T, Simon C, Urassa H, et al. The burden of rabies in Tanzania and its impact on local communities. PLoS Neglected Tropical Diseases. 2013; 7(11): 1-9.
36. Issah B, Ansah T, Alagma H. Awareness of zoonotic diseases among pet owners in wa municipality of ghana. UDS International Journal of Development. 2020; 7(2): 387-97.
37. Hundal JS, Sodhi SS, Gupta A, Singh J, Chahal US. Awareness, knowledge, and risks of zoonotic diseases among livestock farmers in Punjab. Veterinary World. 2016; 9(2): 186-91.
38. Özlü H, Atasever M, Atasever MA. Knowledge, attitude, and practices of cattle farmers regarding zoonotic diseases in Erzurum, Turkey. Austral Journal of Veterinary Sciences. 2020; 52(3): 79-85.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |