Volume 11, Issue 1 (June 2025)
Elderly Health Journal 2025, 11(1): 3-12 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Issazadegan A, Alilou S. Relationships Between Neuroticism and Health Anxiety with Psychosomatic Disorders in the Elderly: Examining the Mediating Role of Rumination. Elderly Health Journal 2025; 11 (1) :3-12
URL: http://ehj.ssu.ac.ir/article-1-337-en.html
URL: http://ehj.ssu.ac.ir/article-1-337-en.html
Department of Psychology, Faculty of Literature and Humanities, Urmia University, Urmia, Iran , a.esazade@gmail.com
Full-Text [PDF 633 kb]
(209 Downloads)
| Abstract (HTML) (700 Views)
Introduction: The present study aimed to model the structural relationships between neuroticism and health anxiety with psychosomatic symptoms in the elderly with psychosomatic disorders, considering the mediating role of rumination.
Methods: This descriptive-correlational research was conducted using structural equation modeling (SEM). The statistical population included elderly individuals visiting medical clinics in Khoy City, Iran. Due to the unavailability of accurate statistics on the elderly population, a convenience sampling method was employed. The sample consisted of 200 elderly individuals who had visited two clinics— Social Security Clinic and the Farhangian Clinic —due to somatic complaints. Data were collected using the Psychosomatic Symptoms Questionnaire, the Health Anxiety Inventory, the Rumination Scale, and the Neuroticism Scale. To investigate the direct and indirect effects among the research variables, Smart PLS software was used for analysis through SEM.
Results: Neuroticism (β = 0.31, t = 6.31) and health anxiety (β = 0.29, t = 5.91) directly predicted psychosomatic disorders in the elderly. Both also significantly predicted rumination (neuroticism β = 0.31, t = 8.70; health anxiety β = 0.59, t = 15.98), which in turn affected psychosomatic disorders (β = 0.37, t = 7.33). Rumination mediated the effects of neuroticism (indirect β = 0.11, t = 5.57) and health anxiety (indirect β = 0.22, t = 6.77). The model showed good fit (SRMR = 0.065, NFI = 0.910).
Conclusion: addressing the psychological aspects of elderly individuals, particularly neuroticism and health anxiety, can significantly improve their physical and mental well-being. Psychological interventions aimed at reducing rumination and enhancing health-related attitudes can effectively prevent and treat psychosomatic disorders. These findings underscore the importance of designing comprehensive intervention programs for the elderly, considering both their psychological and physical dimensions.
Keywords: Psychosomatic Disorders, Disease, Anxiety Disorders, Neuroticism, Rumination, Aging
Copyright © 2025 Elderly Health Journal. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cite.
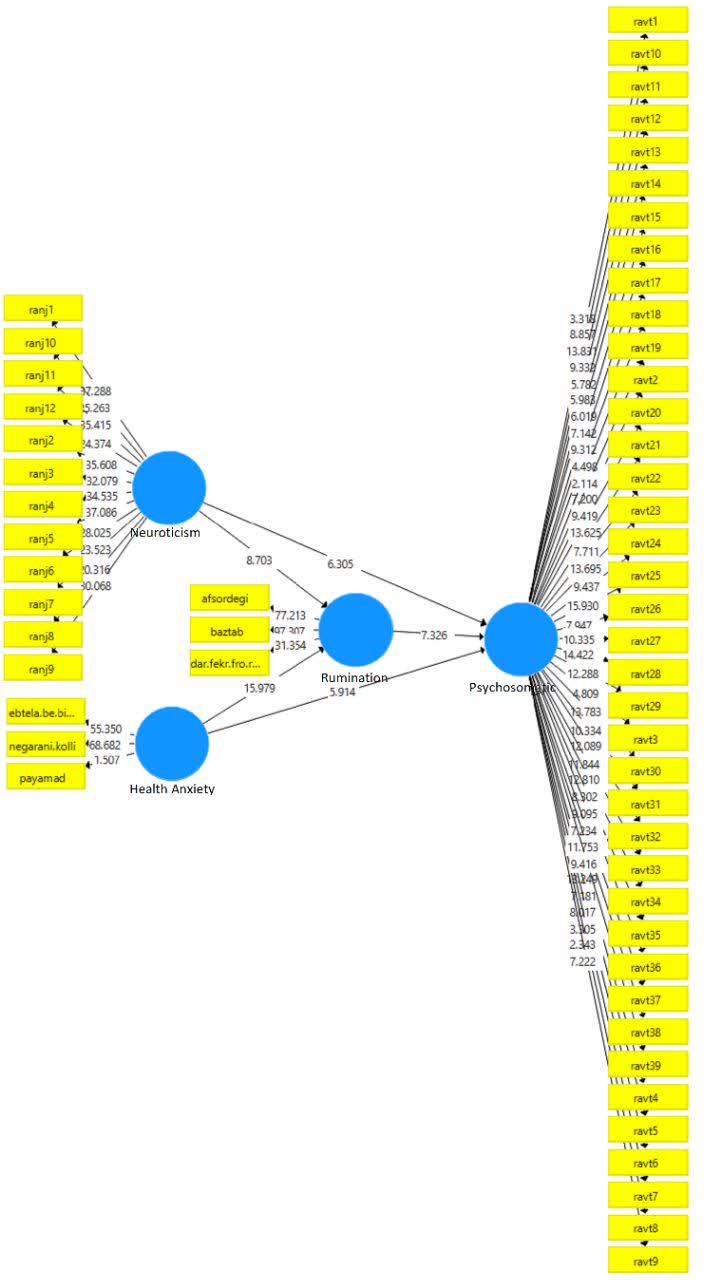
Figure 1. Structural equation model with direct and indirect path coefficient
Full-Text: (189 Views)
Relationships Between Neuroticism and Health Anxiety with Psychosomatic Disorders in the Elderly: Examining the Mediating Role of Rumination
Ali Issazadegan 1*, Shahla Alilou 1
Received 20 Jul 2024
Accepted 24 Nov 2024
A B S T R A C T
Ali Issazadegan 1*, Shahla Alilou 1
- Department of Psychology, Faculty of Literature and Humanities, Urmia University, Urmia, Iran
Received 20 Jul 2024
Accepted 24 Nov 2024
Introduction: The present study aimed to model the structural relationships between neuroticism and health anxiety with psychosomatic symptoms in the elderly with psychosomatic disorders, considering the mediating role of rumination.
Methods: This descriptive-correlational research was conducted using structural equation modeling (SEM). The statistical population included elderly individuals visiting medical clinics in Khoy City, Iran. Due to the unavailability of accurate statistics on the elderly population, a convenience sampling method was employed. The sample consisted of 200 elderly individuals who had visited two clinics— Social Security Clinic and the Farhangian Clinic —due to somatic complaints. Data were collected using the Psychosomatic Symptoms Questionnaire, the Health Anxiety Inventory, the Rumination Scale, and the Neuroticism Scale. To investigate the direct and indirect effects among the research variables, Smart PLS software was used for analysis through SEM.
Results: Neuroticism (β = 0.31, t = 6.31) and health anxiety (β = 0.29, t = 5.91) directly predicted psychosomatic disorders in the elderly. Both also significantly predicted rumination (neuroticism β = 0.31, t = 8.70; health anxiety β = 0.59, t = 15.98), which in turn affected psychosomatic disorders (β = 0.37, t = 7.33). Rumination mediated the effects of neuroticism (indirect β = 0.11, t = 5.57) and health anxiety (indirect β = 0.22, t = 6.77). The model showed good fit (SRMR = 0.065, NFI = 0.910).
Conclusion: addressing the psychological aspects of elderly individuals, particularly neuroticism and health anxiety, can significantly improve their physical and mental well-being. Psychological interventions aimed at reducing rumination and enhancing health-related attitudes can effectively prevent and treat psychosomatic disorders. These findings underscore the importance of designing comprehensive intervention programs for the elderly, considering both their psychological and physical dimensions.
Keywords: Psychosomatic Disorders, Disease, Anxiety Disorders, Neuroticism, Rumination, Aging
Copyright © 2025 Elderly Health Journal. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cite.
Introduction
The aging period is marked by certain physical, social, and psychological characteristics, including a relative decline in physical strength. As age increases, physical abilities gradually diminish (1, 2). Anxiety and depressive disorders are among the most common and severe forms of psychopathology in older adults. They are associated with high levels of distress, reduced quality of life, impaired social adjustment, and an increased risk of suicide (3).
Unfortunately, in many modern societies, the physiological and physical needs of the elderly are often prioritized over their psychological, social, and personality-related needs. Elderly individuals are inherently among the most vulnerable members of society in terms of health status (4). Physical decline, an increase in somatic symptoms, and withdrawal from intensive social and occupational activities lead to preoccupation with illnesses, bodily symptoms, and health-related concerns. Clinical findings highlight the significant role of psychological factors in numerous disorders (5, 6).
Other studies (7, 8) have reported a positive and significant relationship between psychological symptoms and psychosomatic disorders. Psychosomatic disorders manifest as physical symptoms influenced by psychological factors. In recent years, there has been growing global concern about the rising prevalence and rapid progression of psychosomatic disorders. This increase has been attributed to irregular biological conditions and increasingly stressful lifestyles, ultimately leading to dysfunction of vital organs (9).
The term "psychosomatic disorders" or "psychophysiological disorders" refers to physical conditions closely linked to meaningful psychological events (10). These disorders encompass a wide range of conditions, including cardiovascular, respiratory, gastrointestinal, musculoskeletal, urogenital, and dermatological disorders, as well as tension headaches, back pain, neck pain, gastritis, gastric and duodenal ulcers, asthma, cardiovascular diseases, migraines, gastrointestinal issues, and more (11, 12).
Given that psychological states in the elderly, such as prevalent health anxiety, feelings of loneliness, and death anxiety, can influence their physical illnesses and accelerate their progression, addressing their psychological issues is of critical importance (13). As reported in a study (3), heightened personal anxiety is directly linked to emotional, nervous, and psychosomatic disorders. One of the recurring concerns among the elderly is health anxiety (14). Various studies have confirmed the relationship between anxiety and psychosomatic disorders (15, 16), with significant associations reported between somatic symptoms and health anxiety. Similarly, Grönros and Nilsson (16) found that higher levels of psychosomatic symptoms are associated with the persistence of daily anxiety.
Health anxiety, or illness anxiety, is a chronic, episodic, and recurrent condition that often begins in early adulthood and intensifies with age, affecting men and women equally (17). It is characterized by the misinterpretation of bodily sensations or physical changes as symptoms of a severe illness. Those affected by health anxiety become preoccupied with the belief that they are experiencing a physical illness (18, 19). Health anxiety differs from general anxiety in that it involves irrational concern that physical symptoms indicate a severe disease (20).
Salkovskis and Warwick (21) described four maladaptive health-related beliefs critical to understanding health anxiety: the likelihood of having or contracting a disease, the perceived severity of the disease, the inability to cope with the disease, and the inadequacy of medical services for treatment. In its severe form, health anxiety can significantly impact self-assessed mental and physical health and lead to substantial healthcare costs (23, 24). Given the above, health anxiety, as it is associated with high stress levels and obsessive thoughts about illness, can lead to increased worry, stress, and anxiety, potentially resulting in psychosomatic disorders in the elderly.
Many studies have confirmed the relationship between personality factors and psychosomatic disorders. In a study by Ghazanfari et al (25), the relationship between personality traits and psychosomatic disorders was examined, revealing that neuroticism is the strongest predictor of psychosomatic disorders. Other studies have investigated the Big Five personality traits in individuals with psychosomatic disorders and found significant differences in neuroticism and conscientiousness dimensions among these individuals (26, 27). Consequently, neuroticism can be considered another factor associated with psychosomatic disorders.
Neuroticism refers to a tendency to react negatively to various sources of stress. The negative emotions typically associated with this trait include anxiety, fear, irritability, anger, and sadness. In addition to exaggerated negative emotions, neurotic temperament (or neuroticism) is characterized by a pervasive perception that the world is a dangerous and threatening place, accompanied by beliefs about one's inability to manage or cope with challenging events (28). This trait has been identified by researchers as one of the critical factors of personality. Costa and McCrae (29) introduced the Big Five personality traits, which include neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness. These traits appear relatively stable over a lifetime and are valid predictors of emotions and behaviors in various situations (30). Neuroticism is defined as the tendency to experience frequent and intense negative emotions related to a sense of uncontrollability (perceived inadequate coping) in response to stress (28).
Research overwhelmingly highlights the significant impact of neuroticism on general health. For instance, neuroticism is strongly associated with and predicts various mental disorders, including comorbid conditions (31-35). Consequently, both neuroticism and health anxiety are factors linked to high levels of stress, anxiety, and negative emotions (36). Since they are also associated with various physical illnesses and psychological disorders, they may predict psychosomatic disorders in the elderly.
On the other hand, due to age-related circumstances and physical and mental health challenges, elderly individuals often experience repetitive and uncontrollable thoughts about their health. Consequently, rumination may mediate the relationship between neuroticism, health anxiety, and psychosomatic disorders, either amplifying or reducing this association. Rumination acts as a maladaptive cognitive strategy (37). It is a repetitive, involuntary, and often distressing process that can distract individuals from focusing on more important aspects of life (38). Rumination encompasses both automatic, unwanted, and unconscious processes, as well as controlled, deliberate, and conscious thinking. It is typically defined as a repetitive thought pattern revolving around a specific topic (39).
Rumination exacerbates psychological distress. Research findings indicate that it heightens individuals' psychological vulnerability across a wide range of issues, including anxiety, depression, psychosis, insomnia, and impulsive behaviors, by magnifying and prolonging existing negative moods and thoughts (40). These effects may interact with health anxiety and neuroticism, potentially affecting physical health and contributing to psychosomatic disorders. Rumination disrupts functioning, particularly when the mind becomes abnormally and uncontrollably preoccupied. This increases the tendency for mental wandering and escalates rumination (41).
Another study confirmed the link between psychological distress and rumination, reporting significant associations between rumination and anxiety, depression, eating disorders, and more (42). Thus, it can be concluded that rumination, along with the inability to control thoughts, may lead to heightened anxiety and increased neuroticism, creating a foundation for psychosomatic disorders in the elderly.
The elderly population is increasing, expected to rise from 9% to 16% globally and from 6.5% to 17.5% in Iran by 2030 (43, 44). Aging is a complex, ongoing process that requires attention from psychologists (45).
Psychosomatic disorders, health anxiety, and rumination are prevalent issues in old age that cannot be overlooked, especially considering that the elderly constitute a significant portion of society. Examining their psychological and physical problems is of utmost importance. Thus, the present study seeks to investigate whether neuroticism and health anxiety, mediated by rumination, can predict psychosomatic disorders among the elderly.
Methods
Study design
In terms of its objective, this study is classified as applied research. It follows a descriptive-correlational design and aims to model the structural relationships between neuroticism, health anxiety, and psychosomatic disorders in the elderly using Structural Equation Modeling (SEM).
Participants
The study population consisted of elderly individuals who visited Medical Clinics in Khoy City, West Azerbaijan province, Iran. Since an exact list or statistics of elderly clinic visitors was unavailable, a convenience sampling method was employed. The study included participants who voluntarily agreed to participate. Two clinics in Khoy were selected for the study. Elderly patients visiting these clinics with somatic complaints (psychosomatic disorders) were invited to participate in the study. After diagnosing psychosomatic disorders and expressing their willingness, questionnaires were provided to them.
The sample size was determined using the Plante formula for correlational studies, expressed as N≥8M+50N (46). For the present descriptive-correlational study, a minimum sample size of 66 participants was calculated. However, to ensure robustness, 200 participants were recruited.
Inclusion and exclusion criteria
The inclusion criteria were as follows: individuals aged 60 years or older, who expressed willingness and were able to participate in the study. Participants were required to have sufficient literacy to complete the questionnaires and to have visited medical clinics in Khoy within the past six months for psychosomatic complaints. Additionally, participants needed to be free from hereditary, genetic, or chronic illnesses, as well as psychological disorders under active treatment. Information regarding these criteria was obtained through self-reporting by the participants and verification by their attending physicians.
Exclusion criteria included a lack of willingness to cooperate or failure to provide accurate and complete responses to the questionnaires.
Instruments
Psychosomatic Symptoms Questionnaire
This questionnaire, developed by Lockhart et al., (54) aims to assess psychosomatic symptoms. It contains 39 items rated on a 5-point Likert scale, ranging from "very little" (1) to "very much" (5). Items include examples like "dizziness and unreal feelings." The total score is calculated by summing the scores of all items, resulting in a range of 39 to 195. Higher scores indicate higher levels of psychosomatic symptoms and vice versa. Ghasemi et al., (47) evaluated the content, face, and criterion validity of the questionnaire as appropriate. Cronbach's alpha coefficient for this questionnaire was reported above 0.70.
Health Anxiety Inventory (HAI)
This inventory was designed to measure health anxiety. The short form of this questionnaire, developed by Salkovskis et al., (48), consists of 18 items and is commonly referred to as the HAI. Each item includes four options, describing components of health and illness as declarative statements. Participants are required to select the statement that best describes them. The questionnaire has three factors: main section, general health worry, and negative consequences. The subscales include illness onset (items 5, 6, 8, 9, 11, 12), consequences of illness (items 13, 15, 16, 17, 18), and general health worry (items 1, 2, 3, 4, 7, 10, 14). Scoring for each item ranges from 0 to 3, where option A = 0, option B = 1, option C = 2, and option D = 3. The total score ranges from 0 to 54, with a cutoff score of 18. The psychometric properties of this questionnaire have been examined and confirmed in Iran, with Davoudi and Nargassi (49) reporting a validity coefficient of 0.94.
Ruminative Response Scale
This questionnaire was designed and developed by Nolen-Hoeksema and Morrow (50), to measure rumination. It consists of 22 items rated on a 4-point Likert scale (never = 1 to always = 4) and includes items like "You try to analyze your personality to understand why you are depressed." The subscales include reflection (items 7, 11, 12, 20, and 21), brooding (items 5, 10, 13, 15, and 16), and depression (items 1 to 4, 6, 8, 9, 14, 17, 18, 19, and 22). The scores are obtained by summing all 22 items, with a range of 22 to 88. Scores between 22 and 33 indicate low rumination, 33 to 55 indicate moderate rumination, and scores above 55 indicate high rumination. In Iran, Milani and Momeni (51) reported a Cronbach's alpha coefficient of 0.88 as a measure of internal consistency for the Ruminative Response Scale.
Neuroticism Scale
This questionnaire, developed by Costa and McCrae (52), assesses neuroticism and is derived from the 60-item NEO Five-Factor Personality Inventory. It contains 12 items rated on a 5-point Likert scale (strongly disagree = 1 to strongly agree = 5). Items 1, 16, 31, and 46 are reverse-scored. Scores range from 12 to 60, with a cutoff score of 36. The psychometric properties of this questionnaire have been examined and confirmed in Iran (53).
Procedure
This study was conducted under the supervision of Urmia University and at two medical clinics in Khoy city: the Social Security Clinic and the Farhangian Clinic. To initiate the research, an introductory letter was obtained from Urmia University. The selection of medical clinics were based on their specific characteristics, as these centers catered to elderly patients with somatic (psychosomatic) disorders, making them suitable for the study.
Participants were selected from elderly individuals visiting these two medical clinics. A convenience sampling method was used, whereby questionnaires were distributed to elderly individuals who expressed willingness to participate in the study. This sampling method was chosen due to the lack of accurate statistics on the number of elderly patients visiting the clinics and the ease of access to participants. After providing information about the study and obtaining consent forms, the research questionnaires were distributed to the participants.
Statistical analysis
Descriptive statistics, including frequency, percentage, mean, standard deviation, and standard error, were used to summarize the data. For inferential statistics, the SEM was employed to test the research hypotheses. Data analysis was performed using SPSS version 22 and Smart PLS software.
Ethical considerations
Participants in this study faced no physical, financial, or reputational harm. They were given the freedom to withdraw from the study at any time. All collected information was treated as confidential and was never disclosed to anyone. Written consent was obtained from all participants for reviewing their medical records to confirm eligibility.
This study was approved by the Research Ethics Committee of Urmia University under the ethics code IR.AIU.urmia.REC.1402.091. Written informed consent was obtained from all participants.
Results
Descriptive statistics were used to summarize the demographic data, which are presented in Table 1.
Regarding age groups, the highest frequency was observed in the 60-70 years group, with 104 participants (52%). Of them, 142 participants (71%) were married, while 58 participants (29%) were single. Regarding education level, the highest percentage was among those with elementary education, with 96 participants (48%). In terms of specific health conditions, 92 participants (46%) were diagnosed with cardiovascular diseases.
Descriptive characteristics of research variables are presented in Table 2.
Before evaluating the fit of the conceptual model, the data were screened, and outliers were identified using box plots. The assumption of data normality was then tested through the Shapiro-Wilk test, which confirmed that the research variables followed a normal distribution (p > 0.05). The model fit was subsequently assessed at two levels: the measurement model and the structural model.
For the measurement model, convergent validity was evaluated using the Average Variance Extracted (AVE), while reliability was assessed through Cronbach's alpha, Composite Reliability (CR), and the Rho coefficient.
The results, as detailed in Table 3, indicate that all four variables meet the accepted thresholds for these indices. Cronbach's alpha values exceeded the recommended level of 0.7, demonstrating acceptable internal consistency. Similarly, the rho coefficient and CR for all variables were above the acceptable threshold of 0.7, confirming their reliability. Additionally, the AVE values for all variables were greater than 0.5, indicating satisfactory convergent validity. In examining the structural model, the model fit indices including the Standardized Root Mean Square Residual (SRMR) and the Normed Fit Index (NFI) were assessed. The results show that the SRMR is 0.065, which is smaller than the criterion value of 0.08. The NFI is 0.910, which is greater than the criterion value of 0.90. Given that these indices fall within the appropriate range, it can be concluded that the model demonstrates relatively good fit. At the end, the direct and indirect path coefficients, along with the t-values and their significance, are reported. All direct and indirect paths had significant coefficients. These results are presented in Table 4 and Figure 1.
Unfortunately, in many modern societies, the physiological and physical needs of the elderly are often prioritized over their psychological, social, and personality-related needs. Elderly individuals are inherently among the most vulnerable members of society in terms of health status (4). Physical decline, an increase in somatic symptoms, and withdrawal from intensive social and occupational activities lead to preoccupation with illnesses, bodily symptoms, and health-related concerns. Clinical findings highlight the significant role of psychological factors in numerous disorders (5, 6).
Other studies (7, 8) have reported a positive and significant relationship between psychological symptoms and psychosomatic disorders. Psychosomatic disorders manifest as physical symptoms influenced by psychological factors. In recent years, there has been growing global concern about the rising prevalence and rapid progression of psychosomatic disorders. This increase has been attributed to irregular biological conditions and increasingly stressful lifestyles, ultimately leading to dysfunction of vital organs (9).
The term "psychosomatic disorders" or "psychophysiological disorders" refers to physical conditions closely linked to meaningful psychological events (10). These disorders encompass a wide range of conditions, including cardiovascular, respiratory, gastrointestinal, musculoskeletal, urogenital, and dermatological disorders, as well as tension headaches, back pain, neck pain, gastritis, gastric and duodenal ulcers, asthma, cardiovascular diseases, migraines, gastrointestinal issues, and more (11, 12).
Given that psychological states in the elderly, such as prevalent health anxiety, feelings of loneliness, and death anxiety, can influence their physical illnesses and accelerate their progression, addressing their psychological issues is of critical importance (13). As reported in a study (3), heightened personal anxiety is directly linked to emotional, nervous, and psychosomatic disorders. One of the recurring concerns among the elderly is health anxiety (14). Various studies have confirmed the relationship between anxiety and psychosomatic disorders (15, 16), with significant associations reported between somatic symptoms and health anxiety. Similarly, Grönros and Nilsson (16) found that higher levels of psychosomatic symptoms are associated with the persistence of daily anxiety.
Health anxiety, or illness anxiety, is a chronic, episodic, and recurrent condition that often begins in early adulthood and intensifies with age, affecting men and women equally (17). It is characterized by the misinterpretation of bodily sensations or physical changes as symptoms of a severe illness. Those affected by health anxiety become preoccupied with the belief that they are experiencing a physical illness (18, 19). Health anxiety differs from general anxiety in that it involves irrational concern that physical symptoms indicate a severe disease (20).
Salkovskis and Warwick (21) described four maladaptive health-related beliefs critical to understanding health anxiety: the likelihood of having or contracting a disease, the perceived severity of the disease, the inability to cope with the disease, and the inadequacy of medical services for treatment. In its severe form, health anxiety can significantly impact self-assessed mental and physical health and lead to substantial healthcare costs (23, 24). Given the above, health anxiety, as it is associated with high stress levels and obsessive thoughts about illness, can lead to increased worry, stress, and anxiety, potentially resulting in psychosomatic disorders in the elderly.
Many studies have confirmed the relationship between personality factors and psychosomatic disorders. In a study by Ghazanfari et al (25), the relationship between personality traits and psychosomatic disorders was examined, revealing that neuroticism is the strongest predictor of psychosomatic disorders. Other studies have investigated the Big Five personality traits in individuals with psychosomatic disorders and found significant differences in neuroticism and conscientiousness dimensions among these individuals (26, 27). Consequently, neuroticism can be considered another factor associated with psychosomatic disorders.
Neuroticism refers to a tendency to react negatively to various sources of stress. The negative emotions typically associated with this trait include anxiety, fear, irritability, anger, and sadness. In addition to exaggerated negative emotions, neurotic temperament (or neuroticism) is characterized by a pervasive perception that the world is a dangerous and threatening place, accompanied by beliefs about one's inability to manage or cope with challenging events (28). This trait has been identified by researchers as one of the critical factors of personality. Costa and McCrae (29) introduced the Big Five personality traits, which include neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness. These traits appear relatively stable over a lifetime and are valid predictors of emotions and behaviors in various situations (30). Neuroticism is defined as the tendency to experience frequent and intense negative emotions related to a sense of uncontrollability (perceived inadequate coping) in response to stress (28).
Research overwhelmingly highlights the significant impact of neuroticism on general health. For instance, neuroticism is strongly associated with and predicts various mental disorders, including comorbid conditions (31-35). Consequently, both neuroticism and health anxiety are factors linked to high levels of stress, anxiety, and negative emotions (36). Since they are also associated with various physical illnesses and psychological disorders, they may predict psychosomatic disorders in the elderly.
On the other hand, due to age-related circumstances and physical and mental health challenges, elderly individuals often experience repetitive and uncontrollable thoughts about their health. Consequently, rumination may mediate the relationship between neuroticism, health anxiety, and psychosomatic disorders, either amplifying or reducing this association. Rumination acts as a maladaptive cognitive strategy (37). It is a repetitive, involuntary, and often distressing process that can distract individuals from focusing on more important aspects of life (38). Rumination encompasses both automatic, unwanted, and unconscious processes, as well as controlled, deliberate, and conscious thinking. It is typically defined as a repetitive thought pattern revolving around a specific topic (39).
Rumination exacerbates psychological distress. Research findings indicate that it heightens individuals' psychological vulnerability across a wide range of issues, including anxiety, depression, psychosis, insomnia, and impulsive behaviors, by magnifying and prolonging existing negative moods and thoughts (40). These effects may interact with health anxiety and neuroticism, potentially affecting physical health and contributing to psychosomatic disorders. Rumination disrupts functioning, particularly when the mind becomes abnormally and uncontrollably preoccupied. This increases the tendency for mental wandering and escalates rumination (41).
Another study confirmed the link between psychological distress and rumination, reporting significant associations between rumination and anxiety, depression, eating disorders, and more (42). Thus, it can be concluded that rumination, along with the inability to control thoughts, may lead to heightened anxiety and increased neuroticism, creating a foundation for psychosomatic disorders in the elderly.
The elderly population is increasing, expected to rise from 9% to 16% globally and from 6.5% to 17.5% in Iran by 2030 (43, 44). Aging is a complex, ongoing process that requires attention from psychologists (45).
Psychosomatic disorders, health anxiety, and rumination are prevalent issues in old age that cannot be overlooked, especially considering that the elderly constitute a significant portion of society. Examining their psychological and physical problems is of utmost importance. Thus, the present study seeks to investigate whether neuroticism and health anxiety, mediated by rumination, can predict psychosomatic disorders among the elderly.
Methods
Study design
In terms of its objective, this study is classified as applied research. It follows a descriptive-correlational design and aims to model the structural relationships between neuroticism, health anxiety, and psychosomatic disorders in the elderly using Structural Equation Modeling (SEM).
Participants
The study population consisted of elderly individuals who visited Medical Clinics in Khoy City, West Azerbaijan province, Iran. Since an exact list or statistics of elderly clinic visitors was unavailable, a convenience sampling method was employed. The study included participants who voluntarily agreed to participate. Two clinics in Khoy were selected for the study. Elderly patients visiting these clinics with somatic complaints (psychosomatic disorders) were invited to participate in the study. After diagnosing psychosomatic disorders and expressing their willingness, questionnaires were provided to them.
The sample size was determined using the Plante formula for correlational studies, expressed as N≥8M+50N (46). For the present descriptive-correlational study, a minimum sample size of 66 participants was calculated. However, to ensure robustness, 200 participants were recruited.
Inclusion and exclusion criteria
The inclusion criteria were as follows: individuals aged 60 years or older, who expressed willingness and were able to participate in the study. Participants were required to have sufficient literacy to complete the questionnaires and to have visited medical clinics in Khoy within the past six months for psychosomatic complaints. Additionally, participants needed to be free from hereditary, genetic, or chronic illnesses, as well as psychological disorders under active treatment. Information regarding these criteria was obtained through self-reporting by the participants and verification by their attending physicians.
Exclusion criteria included a lack of willingness to cooperate or failure to provide accurate and complete responses to the questionnaires.
Instruments
Psychosomatic Symptoms Questionnaire
This questionnaire, developed by Lockhart et al., (54) aims to assess psychosomatic symptoms. It contains 39 items rated on a 5-point Likert scale, ranging from "very little" (1) to "very much" (5). Items include examples like "dizziness and unreal feelings." The total score is calculated by summing the scores of all items, resulting in a range of 39 to 195. Higher scores indicate higher levels of psychosomatic symptoms and vice versa. Ghasemi et al., (47) evaluated the content, face, and criterion validity of the questionnaire as appropriate. Cronbach's alpha coefficient for this questionnaire was reported above 0.70.
Health Anxiety Inventory (HAI)
This inventory was designed to measure health anxiety. The short form of this questionnaire, developed by Salkovskis et al., (48), consists of 18 items and is commonly referred to as the HAI. Each item includes four options, describing components of health and illness as declarative statements. Participants are required to select the statement that best describes them. The questionnaire has three factors: main section, general health worry, and negative consequences. The subscales include illness onset (items 5, 6, 8, 9, 11, 12), consequences of illness (items 13, 15, 16, 17, 18), and general health worry (items 1, 2, 3, 4, 7, 10, 14). Scoring for each item ranges from 0 to 3, where option A = 0, option B = 1, option C = 2, and option D = 3. The total score ranges from 0 to 54, with a cutoff score of 18. The psychometric properties of this questionnaire have been examined and confirmed in Iran, with Davoudi and Nargassi (49) reporting a validity coefficient of 0.94.
Ruminative Response Scale
This questionnaire was designed and developed by Nolen-Hoeksema and Morrow (50), to measure rumination. It consists of 22 items rated on a 4-point Likert scale (never = 1 to always = 4) and includes items like "You try to analyze your personality to understand why you are depressed." The subscales include reflection (items 7, 11, 12, 20, and 21), brooding (items 5, 10, 13, 15, and 16), and depression (items 1 to 4, 6, 8, 9, 14, 17, 18, 19, and 22). The scores are obtained by summing all 22 items, with a range of 22 to 88. Scores between 22 and 33 indicate low rumination, 33 to 55 indicate moderate rumination, and scores above 55 indicate high rumination. In Iran, Milani and Momeni (51) reported a Cronbach's alpha coefficient of 0.88 as a measure of internal consistency for the Ruminative Response Scale.
Neuroticism Scale
This questionnaire, developed by Costa and McCrae (52), assesses neuroticism and is derived from the 60-item NEO Five-Factor Personality Inventory. It contains 12 items rated on a 5-point Likert scale (strongly disagree = 1 to strongly agree = 5). Items 1, 16, 31, and 46 are reverse-scored. Scores range from 12 to 60, with a cutoff score of 36. The psychometric properties of this questionnaire have been examined and confirmed in Iran (53).
Procedure
This study was conducted under the supervision of Urmia University and at two medical clinics in Khoy city: the Social Security Clinic and the Farhangian Clinic. To initiate the research, an introductory letter was obtained from Urmia University. The selection of medical clinics were based on their specific characteristics, as these centers catered to elderly patients with somatic (psychosomatic) disorders, making them suitable for the study.
Participants were selected from elderly individuals visiting these two medical clinics. A convenience sampling method was used, whereby questionnaires were distributed to elderly individuals who expressed willingness to participate in the study. This sampling method was chosen due to the lack of accurate statistics on the number of elderly patients visiting the clinics and the ease of access to participants. After providing information about the study and obtaining consent forms, the research questionnaires were distributed to the participants.
Statistical analysis
Descriptive statistics, including frequency, percentage, mean, standard deviation, and standard error, were used to summarize the data. For inferential statistics, the SEM was employed to test the research hypotheses. Data analysis was performed using SPSS version 22 and Smart PLS software.
Ethical considerations
Participants in this study faced no physical, financial, or reputational harm. They were given the freedom to withdraw from the study at any time. All collected information was treated as confidential and was never disclosed to anyone. Written consent was obtained from all participants for reviewing their medical records to confirm eligibility.
This study was approved by the Research Ethics Committee of Urmia University under the ethics code IR.AIU.urmia.REC.1402.091. Written informed consent was obtained from all participants.
Results
Descriptive statistics were used to summarize the demographic data, which are presented in Table 1.
Regarding age groups, the highest frequency was observed in the 60-70 years group, with 104 participants (52%). Of them, 142 participants (71%) were married, while 58 participants (29%) were single. Regarding education level, the highest percentage was among those with elementary education, with 96 participants (48%). In terms of specific health conditions, 92 participants (46%) were diagnosed with cardiovascular diseases.
Descriptive characteristics of research variables are presented in Table 2.
Before evaluating the fit of the conceptual model, the data were screened, and outliers were identified using box plots. The assumption of data normality was then tested through the Shapiro-Wilk test, which confirmed that the research variables followed a normal distribution (p > 0.05). The model fit was subsequently assessed at two levels: the measurement model and the structural model.
For the measurement model, convergent validity was evaluated using the Average Variance Extracted (AVE), while reliability was assessed through Cronbach's alpha, Composite Reliability (CR), and the Rho coefficient.
The results, as detailed in Table 3, indicate that all four variables meet the accepted thresholds for these indices. Cronbach's alpha values exceeded the recommended level of 0.7, demonstrating acceptable internal consistency. Similarly, the rho coefficient and CR for all variables were above the acceptable threshold of 0.7, confirming their reliability. Additionally, the AVE values for all variables were greater than 0.5, indicating satisfactory convergent validity. In examining the structural model, the model fit indices including the Standardized Root Mean Square Residual (SRMR) and the Normed Fit Index (NFI) were assessed. The results show that the SRMR is 0.065, which is smaller than the criterion value of 0.08. The NFI is 0.910, which is greater than the criterion value of 0.90. Given that these indices fall within the appropriate range, it can be concluded that the model demonstrates relatively good fit. At the end, the direct and indirect path coefficients, along with the t-values and their significance, are reported. All direct and indirect paths had significant coefficients. These results are presented in Table 4 and Figure 1.
Table 1. Demographic characteristics of participants (n = 200)
Table 2. Descriptive characteristics of the study variables (n = 200)
Table 3. Goodness-of-fit indices of the measurement model
Table 4. Direct and indirect path coefficients
| Descriptive statistics | Variable | ||
| Percentage | Frequency | ||
| 20% | 40 | Under 60 years | Age |
| 45% | 90 | 60 to 70 years | |
| 35% | 70 | Over 70 years | |
| 75% | 150 | Married | Marital status |
| 25% | 50 | Single | |
| 5% | 10 | No formal education | Education |
| 15% | 30 | High school diploma | |
| 20% | 40 | Associate's degree | |
| 30% | 60 | Bachelor's degree | |
| 30% | 60 | Master's degree or higher | |
| 51% | 102 | Cardiovascular diseases | Specific disease |
| 32% | 64 | Diabetes | |
| 24% | 48 | Osteoarthritis | |
Table 2. Descriptive characteristics of the study variables (n = 200)
| Variables | Min. | Max. | Mean | Std. Deviation | Skewness | Kurtosis |
| Rumination | 36 | 87 | 66.15 | 8.58 | -0.33 | 0.13 |
| Neuroticism | 12 | 60 | 40.11 | 11.38 | -0.18 | -0.61 |
| Health anxiety | 10 | 53 | 36.65 | 6.52 | -0.41 | 0.64 |
| Psychosomatic | 71 | 159 | 120.08 | 11.79 | -0.36 | 0.93 |
Table 3. Goodness-of-fit indices of the measurement model
| Variables | Cronbach's alpha | Rho | CR | AVE |
| Rumination | 0.809 | 0.839 | 0.886 | 0.723 |
| Neuroticism | 0.784 | 0.753 | 0.717 | 0.502 |
| Health anxiety | 0.890 | 0.902 | 0.898 | 0.500 |
| Psychosomatic | 0.926 | 0.930 | 0.936 | 0.552 |
Table 4. Direct and indirect path coefficients
| Variables | Mean | Std. Deviation | T-value | Significance |
| Health anxiety → Psychosomatic | 0.29 | 0.49 | 5.91 | 0.001 |
| Health anxiety → Rumination | 0.59 | 0.37 | 15.98 | 0.001 |
| Neuroticism → Psychosomatic | 0.31 | 0.50 | 6.31 | 0.001 |
| Neuroticism → Rumination | 0.31 | 0.36 | 8.70 | 0.001 |
| Rumination → Psychosomatic | 0.37 | 0.51 | 7.33 | 0.001 |
| Health anxiety → Rumination → Psychosomatic | 0.22 | 0.03 | 6.77 | 0.001 |
| Neuroticism → Rumination → Psychosomatic | 0.11 | 0.02 | 5.57 | 0.001 |
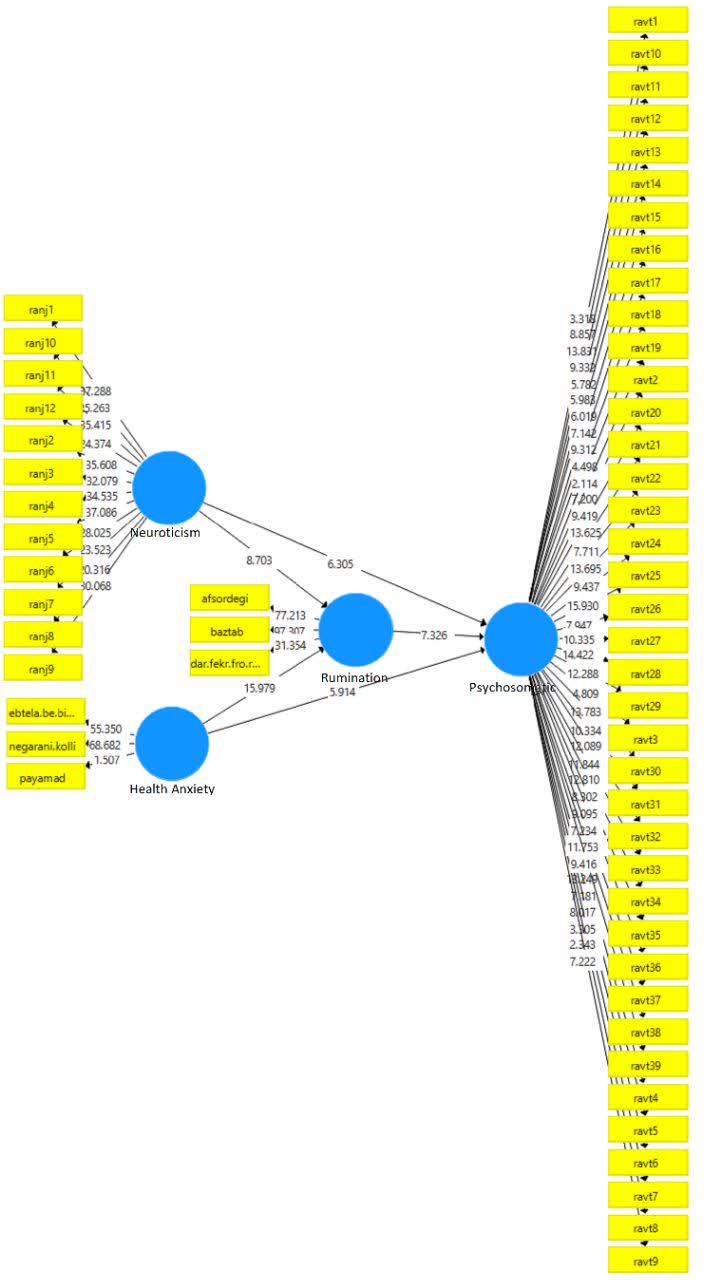
Figure 1. Structural equation model with direct and indirect path coefficient
Discussion
In this study, the structural relationships among neuroticism, health anxiety, and psychosomatic disorders in older adults were examined. The results indicated that both neuroticism and health anxiety, directly and through the mediation of rumination, can serve as significant predictors of psychosomatic disorders in the elderly. These findings underscore the importance of psychological dimensions in older adults’ health and demonstrate that health anxiety and personality traits such as neuroticism can meaningfully influence their physical and mental well-being. Moreover, the results of this study align with previous research (16), emphasizing the importance of managing anxiety and rumination, especially during later life. The following section will discuss the interpretation of the findings, comparison with similar studies, limitations, and recommendations for future research.
The results of this study are consistent with several previous investigations showing that health anxiety and neuroticism can be important predictors of psychosomatic disorders in older adults. For example, Rizal and Susilahati (4) concluded in their research that due to declining physical strength and increased somatic symptoms, older adults are more vulnerable to health anxiety and psychosomatic disorders. These findings mirror those of the current study, which indicates that health anxiety in older adults can influence the onset of psychosomatic disorders. Similarly, Chauhan and Jain (9) emphasized that the prevalence of psychosomatic disorders, particularly in older adults, increases as a result of stress and biological changes. These results also align with the present study, as both health anxiety and neuroticism were directly related to psychosomatic disorders. In addition, Nematillayevna and Temirpulotovich (3) highlighted the association between elevated anxiety and psychosomatic disorders in older adults, noting that health anxiety can lead to both physical and mental problems. These findings are in line with the current study, demonstrating that health anxiety and neuroticism, both directly and through rumination, influence psychosomatic disorders. Taken together, these three studies reinforce the importance of considering psychological dimensions of older adults and their impact on physical health.
To explain these results, it can be stated that neuroticism is a personality trait characterized by a tendency to experience negative emotions and heightened reactivity to stressors (37). Individuals with high neuroticism are more prone to anxiety, fear, irritability, and depression, all of which can threaten their mental and physical health. This personality trait can directly influence the emergence of psychosomatic disorders, as neurotic individuals may readily exhibit physical reactions to stress, including headaches, muscle pain, and gastrointestinal problems (9). Additionally, their elevated anxiety may cause them to misinterpret bodily symptoms as signs of serious illness, a cognitive pattern that can lead to psychosomatic disorders (3).
Regarding health anxiety, this condition can be a key factor in the development of psychosomatic disorders in older adults (4). Health anxiety involves misinterpreting bodily changes as symptoms of severe illnesses, thereby placing significant psychological pressure on individuals, which can ultimately manifest as psychosomatic issues such as migraines, gastrointestinal problems, and cardiovascular complications. One of the previous studies has also shown that health anxiety can have negative effects on mental and physical health, creating persistent worry about one’s well-being (16), which in turn may exacerbate bodily complaints like digestive issues, muscle pain, and headaches.
Finally, rumination, as a repetitive and uncontrollable thought process, can serve as an important mediator in the relationship between neuroticism and health anxiety with psychosomatic disorders (40). Rumination leads individuals to repeatedly focus on problems and negative thoughts, thereby intensifying stress and anxiety, ultimately resulting in psychosomatic disorders (54). In the current study, rumination significantly mediated the relationship between neuroticism and health anxiety with psychosomatic disorders. In other words, individuals exhibiting neurotic traits and health anxiety are more likely to engage in rumination, and this persistent cognitive process can amplify their psychosomatic symptoms. This finding aligns with Seli et al., (41) emphasizing that rumination can increase individuals’ psychological vulnerability to both physical and mental health issues.
The findings of this research highlight the importance of paying attention to the psychological characteristics of older adults. In particular, therapeutic interventions for the elderly should include strategies aimed at reducing health anxiety, neuroticism, and rumination. Interventions such as cognitive-behavioral therapy can be effective in reducing health-related worries and altering negative thought patters (54). Theoretically, this study contributes to a better understanding of the relationship between personality traits, health anxiety, and psychosomatic disorders, and facilitates the development of psychological models that incorporate rumination as a mediating variable.
Conclusion
The present study examined the structural relationships among neuroticism, health anxiety, and psychosomatic disorders in older adults, demonstrating that both psychological variables, particularly through the mediation of rumination, exert a significant influence on the onset of psychosomatic disorders. These findings indicate that older adults with higher levels of neuroticism and health anxiety are at greater risk for developing psychosomatic health problems. Moreover, the mediating role of rumination underscores the importance of addressing cognitive processes in the treatment of these disorders. From a theoretical perspective, the results of this research enrich psychological models related to the mental health of older adults and highlight the need to consider personality traits and anxiety in treatment plans. Practically, this study may guide the development of psychological interventions aimed at reducing health anxiety and rumination, especially for older adults suffering from psychosomatic disorders. Ultimately, the findings encourage researchers and health professionals to integrate psychological and cognitive interventions for the prevention and treatment of psychosomatic disorders in older populations.
Study limitations
This study has certain limitations that should be taken into account. One major limitation is that the sample consisted only of older adults who visited medical clinics in the city of Khoy, limiting the generalizability of the findings to other regions or populations of older adults. Additionally, accessing all older adults with psychosomatic disorders in the broader community posed challenges, especially given that participants were primarily recruited from two clinics. The relatively small sample size (200 individuals) further restricts the generalization of the results to larger populations. Moreover, the use of convenience sampling means that the findings may not fully represent the demographic characteristics and personal experiences of older adults with psychosomatic disorders. The use of self-report measures and the absence of a neutral control condition also may have influenced the validity of the results.
Conflict of Interest
The authors have no financial or personal conflicts of interest to declare.
Acknowledgments
We extend our sincere gratitude to all the older adults and their families who dedicated their time and effort to participate in this research. We also appreciate the cooperation of the medical centers in the city of Khoy—particularly the Social Security Clinic and the Farhangian Clinic—that played a crucial role in facilitating the data collection process.
Funding
This research was conducted under the supervision and support of the Urmia University. The researchers received no external funding for this study.
Authors’ contributions
The design and conceptualization of the study were carried out by Alilou and Issazadegan. Alilou was responsible for data collection, conducting the initial data analyses, and drafting the manuscript. Issazadegan provided overall supervision of all study stages and the data analysis process and offered feedback to improve methodology and statistical analyses. Both authors approved the final version of the manuscript.
References
1. Khalili Z, Jafarizadeh M, Mohammadi S, Molaei B, Ebrahimi Belil F. Neglect in nursing homes: prevalence and risk factors. Elderly Health Journal. 2024; 10(1): 14-9.
2. Ibrahim RM, Ahmed MM, Younis NM. Correlation between physical activity and quality of life of elderly. Current Clinical and Medical Education. 2024; 2(8): 9-17.
3. Nematillayevna SD, Temirpulotovich TB. Prevalence of anxiety and depressive disorders in elderly patients. Scientific Journal of Applied and Medical Sciences. 2024; 3(2): 118-23.
4. Rizal A, Susilahati S. Implementation of the Jakarta elderly card program in meeting the basic needs of the elderly. Riwayat: Educational Journal of History and Humanities. 2023; 6(2): 596-605.
5. Nisar H, Srivastava R. Fundamental concept of psychosomatic disorders: a review. International Journal of Contemporary Medicine Surgery and Radiology. 2018; 3(1): 12-8.
6. Spytska L. Social and psychological problems of the elderly in the modern society. Scientific World Journal. 2023; 30(18-03): 108-12.
7. Hange D, Bengtsson C, Sundh V, Björkelund C. The natural history of psychosomatic symptoms and their association with psychological symptoms: observations from the Population Study of Women in Gothenburg. The European Journal of General Practice. 2007; 13(2): 60-6.
8. Smakowski AL, Hüsing P, Völcker S, Löwe B, Rosmalen JG, Shedden-Mora M, et al. Psychological risk factors of somatic symptom disorder: A systematic review and meta-analysis of cross-sectional and longitudinal studies. Journal of Psychosomatic Research. 2024; 181: 111608.
9. Chauhan A, Jain CK. Psychosomatic disorder: the current implications and challenges. Cardiovascular & Hematological Agents in Medicinal Chemistry. 2024; 22(4): 399-406.
10. Dash S. Psycosomatic disorders an overall review on oral manifestations. Journal of Dentistry and Dental Materials. 2024; 2(1): 1-5.
11. Abdivalyevna AN, Abdukhamid AF. Factors causing personal psychosomatic disorders. International Journal of Advance Scientific Research. 2023; 3(11): 343-7.
12. Philippova A, Malkina O, Korotun V, Shatova E. The role of somatic factors in early childhood and adolescent psychosomatic disorders. Bangladesh Journal of Medical Science. 2023; 22(3): 687-94.
13. Looper KJ, Kirmayer LJ. Hypochondriacal concerns in a community population. Psychological Medicine. 2001; 31(4): 577-84.
14. Yildirim H, Işik K, Aylaz R. The effect of anxiety levels of elderly people in quarantine on depression during covid-19 pandemic. Social Work in Public Health. 2021; 36(2): 194-204.
15. Müller M, Jürgens J, Redaèlli M, Klingberg K, Hautz WE, Stock S. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. 2018; 8(8): 1-10.
16. Grönros J, Nilsson EH, Köteles F, Nordin S. Association between somatic symptoms and modern health worries. Journal of Psychosomatic Research. 2020; 135: 110163.
17. Association AP. The practice of electroconvulsive therapy: recommendations for treatment, training, and privileging (A task force report of the American Psychiatric Association): American Psychiatric Publication; 2024.
18. Fergusson-White CA. Self-regulation in multiple sclerosis: the role of illness cognitions and coping in adjustment [PhD thesis]. Stirling: University of Stirling; 2008.
19. Sauer KS, Witthöft M, Rief W. Somatic symptom disorder and health anxiety: assessment and management. Neurologic Clinics. 2023; 41(4): 745-58.
20. Diamond PR, Dysch L, Daniels J. Health anxiety in stroke survivors: a cross-sectional study on the prevalence of health anxiety in stroke survivors and its impact on quality of life. Disability and Rehabilitation. 2023; 45(1): 27-33.
21. Salkovskis PM, Warwick HM. Morbid preoccupations, health anxiety and reassurance: a cognitive-behavioural approach to hypochondriasis. Behaviour Research and Therapy. 1986; 24(5): 597-602.
22. Windsor NA, Li SH, Joubert A, Upton E, Moulds M, Newby JM. Intrusive thoughts and images in health anxiety: rates, characteristics, and responses. Clinical Psychology & Psychotherapy. 2024; 31(6): 70017.
23. Fink P, Ørnbøl E, Christensen KS. The outcome of health anxiety in primary care. A two-year follow-up study on health care costs and self-rated health. PloS One. 2010; 5(3): 1-12.
24. Mahoney AE, Dobinson K, Millard M, Newby JM. A clinician’s quick guide to evidence-based approaches: health anxiety. Clinical Psychologist. 2024; 1-3.
25. Ghazanfari E, Kazemnejad A, Feizi A, Fesharaki MG, Dinu I, Keshteli AH, et al. The relationship between personality traits and psychosomatic complaints in a sample of Iranian adults. Journal of Affective Disorders. 2020; 261: 253-8.
26. Abdolkarimi M, Sadeghi-Yarandi M, Sakari P. Investigating the relationship between personality traits of hardiness and perfectionism with stress and psychosomatic symptoms: a cross-sectional study among nurses in Iran. BMC Psychology. 2024; 12(1): 1-10.
27. Schmitz N, Hartkamp N, Baldini C, Rollnik J, Tress W. Psychometric properties of the German version of the NEO-FFI in psychosomatic outpatients. Personality and Individual Differences. 2001; 31(5): 713-22.
28. Barlow DH, Ellard KK, Sauer-Zavala S, Bullis JR, Carl JR. The origins of neuroticism. Perspectives on Psychological Science. 2014; 9(5): 481-96.
In this study, the structural relationships among neuroticism, health anxiety, and psychosomatic disorders in older adults were examined. The results indicated that both neuroticism and health anxiety, directly and through the mediation of rumination, can serve as significant predictors of psychosomatic disorders in the elderly. These findings underscore the importance of psychological dimensions in older adults’ health and demonstrate that health anxiety and personality traits such as neuroticism can meaningfully influence their physical and mental well-being. Moreover, the results of this study align with previous research (16), emphasizing the importance of managing anxiety and rumination, especially during later life. The following section will discuss the interpretation of the findings, comparison with similar studies, limitations, and recommendations for future research.
The results of this study are consistent with several previous investigations showing that health anxiety and neuroticism can be important predictors of psychosomatic disorders in older adults. For example, Rizal and Susilahati (4) concluded in their research that due to declining physical strength and increased somatic symptoms, older adults are more vulnerable to health anxiety and psychosomatic disorders. These findings mirror those of the current study, which indicates that health anxiety in older adults can influence the onset of psychosomatic disorders. Similarly, Chauhan and Jain (9) emphasized that the prevalence of psychosomatic disorders, particularly in older adults, increases as a result of stress and biological changes. These results also align with the present study, as both health anxiety and neuroticism were directly related to psychosomatic disorders. In addition, Nematillayevna and Temirpulotovich (3) highlighted the association between elevated anxiety and psychosomatic disorders in older adults, noting that health anxiety can lead to both physical and mental problems. These findings are in line with the current study, demonstrating that health anxiety and neuroticism, both directly and through rumination, influence psychosomatic disorders. Taken together, these three studies reinforce the importance of considering psychological dimensions of older adults and their impact on physical health.
To explain these results, it can be stated that neuroticism is a personality trait characterized by a tendency to experience negative emotions and heightened reactivity to stressors (37). Individuals with high neuroticism are more prone to anxiety, fear, irritability, and depression, all of which can threaten their mental and physical health. This personality trait can directly influence the emergence of psychosomatic disorders, as neurotic individuals may readily exhibit physical reactions to stress, including headaches, muscle pain, and gastrointestinal problems (9). Additionally, their elevated anxiety may cause them to misinterpret bodily symptoms as signs of serious illness, a cognitive pattern that can lead to psychosomatic disorders (3).
Regarding health anxiety, this condition can be a key factor in the development of psychosomatic disorders in older adults (4). Health anxiety involves misinterpreting bodily changes as symptoms of severe illnesses, thereby placing significant psychological pressure on individuals, which can ultimately manifest as psychosomatic issues such as migraines, gastrointestinal problems, and cardiovascular complications. One of the previous studies has also shown that health anxiety can have negative effects on mental and physical health, creating persistent worry about one’s well-being (16), which in turn may exacerbate bodily complaints like digestive issues, muscle pain, and headaches.
Finally, rumination, as a repetitive and uncontrollable thought process, can serve as an important mediator in the relationship between neuroticism and health anxiety with psychosomatic disorders (40). Rumination leads individuals to repeatedly focus on problems and negative thoughts, thereby intensifying stress and anxiety, ultimately resulting in psychosomatic disorders (54). In the current study, rumination significantly mediated the relationship between neuroticism and health anxiety with psychosomatic disorders. In other words, individuals exhibiting neurotic traits and health anxiety are more likely to engage in rumination, and this persistent cognitive process can amplify their psychosomatic symptoms. This finding aligns with Seli et al., (41) emphasizing that rumination can increase individuals’ psychological vulnerability to both physical and mental health issues.
The findings of this research highlight the importance of paying attention to the psychological characteristics of older adults. In particular, therapeutic interventions for the elderly should include strategies aimed at reducing health anxiety, neuroticism, and rumination. Interventions such as cognitive-behavioral therapy can be effective in reducing health-related worries and altering negative thought patters (54). Theoretically, this study contributes to a better understanding of the relationship between personality traits, health anxiety, and psychosomatic disorders, and facilitates the development of psychological models that incorporate rumination as a mediating variable.
Conclusion
The present study examined the structural relationships among neuroticism, health anxiety, and psychosomatic disorders in older adults, demonstrating that both psychological variables, particularly through the mediation of rumination, exert a significant influence on the onset of psychosomatic disorders. These findings indicate that older adults with higher levels of neuroticism and health anxiety are at greater risk for developing psychosomatic health problems. Moreover, the mediating role of rumination underscores the importance of addressing cognitive processes in the treatment of these disorders. From a theoretical perspective, the results of this research enrich psychological models related to the mental health of older adults and highlight the need to consider personality traits and anxiety in treatment plans. Practically, this study may guide the development of psychological interventions aimed at reducing health anxiety and rumination, especially for older adults suffering from psychosomatic disorders. Ultimately, the findings encourage researchers and health professionals to integrate psychological and cognitive interventions for the prevention and treatment of psychosomatic disorders in older populations.
Study limitations
This study has certain limitations that should be taken into account. One major limitation is that the sample consisted only of older adults who visited medical clinics in the city of Khoy, limiting the generalizability of the findings to other regions or populations of older adults. Additionally, accessing all older adults with psychosomatic disorders in the broader community posed challenges, especially given that participants were primarily recruited from two clinics. The relatively small sample size (200 individuals) further restricts the generalization of the results to larger populations. Moreover, the use of convenience sampling means that the findings may not fully represent the demographic characteristics and personal experiences of older adults with psychosomatic disorders. The use of self-report measures and the absence of a neutral control condition also may have influenced the validity of the results.
Conflict of Interest
The authors have no financial or personal conflicts of interest to declare.
Acknowledgments
We extend our sincere gratitude to all the older adults and their families who dedicated their time and effort to participate in this research. We also appreciate the cooperation of the medical centers in the city of Khoy—particularly the Social Security Clinic and the Farhangian Clinic—that played a crucial role in facilitating the data collection process.
Funding
This research was conducted under the supervision and support of the Urmia University. The researchers received no external funding for this study.
Authors’ contributions
The design and conceptualization of the study were carried out by Alilou and Issazadegan. Alilou was responsible for data collection, conducting the initial data analyses, and drafting the manuscript. Issazadegan provided overall supervision of all study stages and the data analysis process and offered feedback to improve methodology and statistical analyses. Both authors approved the final version of the manuscript.
References
1. Khalili Z, Jafarizadeh M, Mohammadi S, Molaei B, Ebrahimi Belil F. Neglect in nursing homes: prevalence and risk factors. Elderly Health Journal. 2024; 10(1): 14-9.
2. Ibrahim RM, Ahmed MM, Younis NM. Correlation between physical activity and quality of life of elderly. Current Clinical and Medical Education. 2024; 2(8): 9-17.
3. Nematillayevna SD, Temirpulotovich TB. Prevalence of anxiety and depressive disorders in elderly patients. Scientific Journal of Applied and Medical Sciences. 2024; 3(2): 118-23.
4. Rizal A, Susilahati S. Implementation of the Jakarta elderly card program in meeting the basic needs of the elderly. Riwayat: Educational Journal of History and Humanities. 2023; 6(2): 596-605.
5. Nisar H, Srivastava R. Fundamental concept of psychosomatic disorders: a review. International Journal of Contemporary Medicine Surgery and Radiology. 2018; 3(1): 12-8.
6. Spytska L. Social and psychological problems of the elderly in the modern society. Scientific World Journal. 2023; 30(18-03): 108-12.
7. Hange D, Bengtsson C, Sundh V, Björkelund C. The natural history of psychosomatic symptoms and their association with psychological symptoms: observations from the Population Study of Women in Gothenburg. The European Journal of General Practice. 2007; 13(2): 60-6.
8. Smakowski AL, Hüsing P, Völcker S, Löwe B, Rosmalen JG, Shedden-Mora M, et al. Psychological risk factors of somatic symptom disorder: A systematic review and meta-analysis of cross-sectional and longitudinal studies. Journal of Psychosomatic Research. 2024; 181: 111608.
9. Chauhan A, Jain CK. Psychosomatic disorder: the current implications and challenges. Cardiovascular & Hematological Agents in Medicinal Chemistry. 2024; 22(4): 399-406.
10. Dash S. Psycosomatic disorders an overall review on oral manifestations. Journal of Dentistry and Dental Materials. 2024; 2(1): 1-5.
11. Abdivalyevna AN, Abdukhamid AF. Factors causing personal psychosomatic disorders. International Journal of Advance Scientific Research. 2023; 3(11): 343-7.
12. Philippova A, Malkina O, Korotun V, Shatova E. The role of somatic factors in early childhood and adolescent psychosomatic disorders. Bangladesh Journal of Medical Science. 2023; 22(3): 687-94.
13. Looper KJ, Kirmayer LJ. Hypochondriacal concerns in a community population. Psychological Medicine. 2001; 31(4): 577-84.
14. Yildirim H, Işik K, Aylaz R. The effect of anxiety levels of elderly people in quarantine on depression during covid-19 pandemic. Social Work in Public Health. 2021; 36(2): 194-204.
15. Müller M, Jürgens J, Redaèlli M, Klingberg K, Hautz WE, Stock S. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. 2018; 8(8): 1-10.
16. Grönros J, Nilsson EH, Köteles F, Nordin S. Association between somatic symptoms and modern health worries. Journal of Psychosomatic Research. 2020; 135: 110163.
17. Association AP. The practice of electroconvulsive therapy: recommendations for treatment, training, and privileging (A task force report of the American Psychiatric Association): American Psychiatric Publication; 2024.
18. Fergusson-White CA. Self-regulation in multiple sclerosis: the role of illness cognitions and coping in adjustment [PhD thesis]. Stirling: University of Stirling; 2008.
19. Sauer KS, Witthöft M, Rief W. Somatic symptom disorder and health anxiety: assessment and management. Neurologic Clinics. 2023; 41(4): 745-58.
20. Diamond PR, Dysch L, Daniels J. Health anxiety in stroke survivors: a cross-sectional study on the prevalence of health anxiety in stroke survivors and its impact on quality of life. Disability and Rehabilitation. 2023; 45(1): 27-33.
21. Salkovskis PM, Warwick HM. Morbid preoccupations, health anxiety and reassurance: a cognitive-behavioural approach to hypochondriasis. Behaviour Research and Therapy. 1986; 24(5): 597-602.
22. Windsor NA, Li SH, Joubert A, Upton E, Moulds M, Newby JM. Intrusive thoughts and images in health anxiety: rates, characteristics, and responses. Clinical Psychology & Psychotherapy. 2024; 31(6): 70017.
23. Fink P, Ørnbøl E, Christensen KS. The outcome of health anxiety in primary care. A two-year follow-up study on health care costs and self-rated health. PloS One. 2010; 5(3): 1-12.
24. Mahoney AE, Dobinson K, Millard M, Newby JM. A clinician’s quick guide to evidence-based approaches: health anxiety. Clinical Psychologist. 2024; 1-3.
25. Ghazanfari E, Kazemnejad A, Feizi A, Fesharaki MG, Dinu I, Keshteli AH, et al. The relationship between personality traits and psychosomatic complaints in a sample of Iranian adults. Journal of Affective Disorders. 2020; 261: 253-8.
26. Abdolkarimi M, Sadeghi-Yarandi M, Sakari P. Investigating the relationship between personality traits of hardiness and perfectionism with stress and psychosomatic symptoms: a cross-sectional study among nurses in Iran. BMC Psychology. 2024; 12(1): 1-10.
27. Schmitz N, Hartkamp N, Baldini C, Rollnik J, Tress W. Psychometric properties of the German version of the NEO-FFI in psychosomatic outpatients. Personality and Individual Differences. 2001; 31(5): 713-22.
28. Barlow DH, Ellard KK, Sauer-Zavala S, Bullis JR, Carl JR. The origins of neuroticism. Perspectives on Psychological Science. 2014; 9(5): 481-96.
29. Costa PT, Robert R. Revised NEO personality inventory (NEO PI-R) and NEO five-factor inventory (neo-ffi). Psychological Assessment Resource, 1992.
30. Schultz DP, Schultz SE. Theories of personality. 11th ed. Cengage Learning: Thomson; 2005.
31. Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. The British Journal of Psychiatry. 2005; 186(3): 190-6.
32. Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006; 2(1): 111-33.
33. Weinstock LM, Whisman MA. Neuroticism as a common feature of the depressive and anxiety disorders: a test of the revised integrative hierarchical model in a national sample. Journal of Abnormal Psychology. 2006; 115(1): 68-74.
34. Xia D, Han X, Zeng Y, Wang J, Xu K, Zhang T, et al. Disease trajectory of high neuroticism and the relevance to psychiatric disorders: a retro-prospective cohort study. Acta Psychiatrica Scandinavica. 2024; 149(2): 133-46.
35. Chen YN. The relationship between personality traits, emotional stability and mental health in art vocational and technical college students during epidemic prevention and control. Psychology Research and Behavior Management. 2023; 16: 2857-67.
36. Feist J, Feist GJ, Roberts TA. Theories of personality. 10th ed. Yogyakarta: Pustaka Pelajar; 2008.
37. Smith KE, Mason TB, Lavender JM. Rumination and eating disorder psychopathology: A meta-analysis. Clinical Psychology Review. 2018; 61: 9-23.
38. Li T, Liu T, Han J, Zhang M, Li Z, Zhu Q, et al. The relationship among resilience, rumination and posttraumatic growth in hemodialysis patients in North China. Psychology, Health & Medicine. 2018 Apr 21; 23(4):442-53.
39. Van Natta O. From the Slime and Mud: Rumination as Fuel for Artistic Process [Master thesis]. Florida: University of Central Florida; 2024.
40. Watkins ER, Roberts H. Reflecting on rumination: consequences, causes, mechanisms and treatment of rumination. Behaviour Research and Therapy. 2020; 127: 103573.
41. Seli P, Risko EF, Smilek D, Schacter DL. Mind-wandering with and without intention. Trends in Cognitive Sciences. 2016; 20(8): 605-17.
42. Rickerby N, Krug I, Fuller-Tyszkiewicz M, Forte E, Davenport R, Chayadi E, et al. Rumination across depression, anxiety, and eating disorders in adults: a meta-analytic review. Clinical Psychology: Science and Practice. 2024; 31(2): 25-68.
43. Hwang J, Park S. Gender-specific prevalence and risk factors of sarcopenic obesity in the Korean elderly population: a nationwide cross-sectional study. International Journal of Environmental Research and Public Health. 2023; 20(2): 1-9.
44. Marsa R, Younesi SJ, Barekati S, Ramshini M, Ghyasi H. A Comparative study on stress, anxiety and depression between nursing-home elderly residents and home-dwelling elderly people. Salmand: Iranian Journal of Ageing. 2020; 15(58): 176-87. [Persian]
45. Younis NM, Ibrahim RM, Ahmed MM. Health problems related to quality of life among aging in Iraq. Journal of Current Medical Research and Opinion. 2024; 7(06): 3015-24.
46. Pallant J. SPSS survival manual: A step-by-step guide to data analysis using IBM SPSS. 7th ed. London: Routledge; 2020.
47. Ghasemi E, Zeinab A, Azam N, Ali EM. Prediction of school burnout based on psychosomatic symptoms, personality traits, father-child interaction and its components in students. Rooyesh-e-Ravanshenasi. 2024; 13(6): 191-200. [Persian]
48. Salkovskis PM, Rimes KA, Warwick HM, Clark D. The health anxiety inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine. 2002; 32(5): 843-53.
49. Davoudi I, Nargassi F, Mehrabizadeh M. Gender differences in health anxiety and related dysfunctional beliefs: Controlling for age. Quarterly Journal of Health Psychology. 2012; 1(3): 1-9. [Persian]
50. Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. Journal of Personality and Social Psychology. 1991; 61(1): 115-21.
51. Milani FB, Momeni K, Dehghani-Arani F, Beyramvand Y, Setoudehmaram S, Saffarifard R. The mediating role of rumination in the relationship between high school students with borderline personality disorder and self-injury. Journal of Applied Psycology Research. 2023; 14(1): 85-98. [Persian]
52. Costa PT, McCrae RR. The revised neo personality inventory (NEO-PI-R). In Boyle JG, Matthews G, Saklofske DH, editors. The SAGE handbook of personality theory and assessment. Vol. 2. Personality measurement and testing. Sage Publications, Inc; 2008. p.179-98.
53. Azkhosh M, Asgari A. Five factor model in Iranian culture: A psychometrics analysis of NEO-five factor inventory (NEO-FFI). International Journal of Indian Psychology. 2014; 1(4): 1-24.
54. Lockhart G, MacKinnon DP, Ohlrich V. Mediation analysis in psychosomatic medicine research. Psychosomatic medicine. 2011; 73(1): 29-43.
31. Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. The British Journal of Psychiatry. 2005; 186(3): 190-6.
32. Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006; 2(1): 111-33.
33. Weinstock LM, Whisman MA. Neuroticism as a common feature of the depressive and anxiety disorders: a test of the revised integrative hierarchical model in a national sample. Journal of Abnormal Psychology. 2006; 115(1): 68-74.
34. Xia D, Han X, Zeng Y, Wang J, Xu K, Zhang T, et al. Disease trajectory of high neuroticism and the relevance to psychiatric disorders: a retro-prospective cohort study. Acta Psychiatrica Scandinavica. 2024; 149(2): 133-46.
35. Chen YN. The relationship between personality traits, emotional stability and mental health in art vocational and technical college students during epidemic prevention and control. Psychology Research and Behavior Management. 2023; 16: 2857-67.
36. Feist J, Feist GJ, Roberts TA. Theories of personality. 10th ed. Yogyakarta: Pustaka Pelajar; 2008.
37. Smith KE, Mason TB, Lavender JM. Rumination and eating disorder psychopathology: A meta-analysis. Clinical Psychology Review. 2018; 61: 9-23.
38. Li T, Liu T, Han J, Zhang M, Li Z, Zhu Q, et al. The relationship among resilience, rumination and posttraumatic growth in hemodialysis patients in North China. Psychology, Health & Medicine. 2018 Apr 21; 23(4):442-53.
39. Van Natta O. From the Slime and Mud: Rumination as Fuel for Artistic Process [Master thesis]. Florida: University of Central Florida; 2024.
40. Watkins ER, Roberts H. Reflecting on rumination: consequences, causes, mechanisms and treatment of rumination. Behaviour Research and Therapy. 2020; 127: 103573.
41. Seli P, Risko EF, Smilek D, Schacter DL. Mind-wandering with and without intention. Trends in Cognitive Sciences. 2016; 20(8): 605-17.
42. Rickerby N, Krug I, Fuller-Tyszkiewicz M, Forte E, Davenport R, Chayadi E, et al. Rumination across depression, anxiety, and eating disorders in adults: a meta-analytic review. Clinical Psychology: Science and Practice. 2024; 31(2): 25-68.
43. Hwang J, Park S. Gender-specific prevalence and risk factors of sarcopenic obesity in the Korean elderly population: a nationwide cross-sectional study. International Journal of Environmental Research and Public Health. 2023; 20(2): 1-9.
44. Marsa R, Younesi SJ, Barekati S, Ramshini M, Ghyasi H. A Comparative study on stress, anxiety and depression between nursing-home elderly residents and home-dwelling elderly people. Salmand: Iranian Journal of Ageing. 2020; 15(58): 176-87. [Persian]
45. Younis NM, Ibrahim RM, Ahmed MM. Health problems related to quality of life among aging in Iraq. Journal of Current Medical Research and Opinion. 2024; 7(06): 3015-24.
46. Pallant J. SPSS survival manual: A step-by-step guide to data analysis using IBM SPSS. 7th ed. London: Routledge; 2020.
47. Ghasemi E, Zeinab A, Azam N, Ali EM. Prediction of school burnout based on psychosomatic symptoms, personality traits, father-child interaction and its components in students. Rooyesh-e-Ravanshenasi. 2024; 13(6): 191-200. [Persian]
48. Salkovskis PM, Rimes KA, Warwick HM, Clark D. The health anxiety inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine. 2002; 32(5): 843-53.
49. Davoudi I, Nargassi F, Mehrabizadeh M. Gender differences in health anxiety and related dysfunctional beliefs: Controlling for age. Quarterly Journal of Health Psychology. 2012; 1(3): 1-9. [Persian]
50. Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. Journal of Personality and Social Psychology. 1991; 61(1): 115-21.
51. Milani FB, Momeni K, Dehghani-Arani F, Beyramvand Y, Setoudehmaram S, Saffarifard R. The mediating role of rumination in the relationship between high school students with borderline personality disorder and self-injury. Journal of Applied Psycology Research. 2023; 14(1): 85-98. [Persian]
52. Costa PT, McCrae RR. The revised neo personality inventory (NEO-PI-R). In Boyle JG, Matthews G, Saklofske DH, editors. The SAGE handbook of personality theory and assessment. Vol. 2. Personality measurement and testing. Sage Publications, Inc; 2008. p.179-98.
53. Azkhosh M, Asgari A. Five factor model in Iranian culture: A psychometrics analysis of NEO-five factor inventory (NEO-FFI). International Journal of Indian Psychology. 2014; 1(4): 1-24.
54. Lockhart G, MacKinnon DP, Ohlrich V. Mediation analysis in psychosomatic medicine research. Psychosomatic medicine. 2011; 73(1): 29-43.
Type of Study: Research |
Subject:
Special
Received: 2024/11/8 | Accepted: 2024/12/18 | Published: 2025/06/20
Received: 2024/11/8 | Accepted: 2024/12/18 | Published: 2025/06/20
References
1. Khalili Z, Jafarizadeh M, Mohammadi S, Molaei B, Ebrahimi Belil F. Neglect in nursing homes: prevalence and risk factors. Elderly Health Journal. 2024; 10(1): 14-9.
2. Ibrahim RM, Ahmed MM, Younis NM. Correlation between physical activity and quality of life of elderly. Current Clinical and Medical Education. 2024; 2(8): 9-17.
3. Nematillayevna SD, Temirpulotovich TB. Prevalence of anxiety and depressive disorders in elderly patients. Scientific Journal of Applied and Medical Sciences. 2024; 3(2): 118-23.
4. Rizal A, Susilahati S. Implementation of the Jakarta elderly card program in meeting the basic needs of the elderly. Riwayat: Educational Journal of History and Humanities. 2023; 6(2): 596-605.
5. Nisar H, Srivastava R. Fundamental concept of psychosomatic disorders: a review. International Journal of Contemporary Medicine Surgery and Radiology. 2018; 3(1): 12-8.
6. Spytska L. Social and psychological problems of the elderly in the modern society. Scientific World Journal. 2023; 30(18-03): 108-12.
7. Hange D, Bengtsson C, Sundh V, Björkelund C. The natural history of psychosomatic symptoms and their association with psychological symptoms: observations from the Population Study of Women in Gothenburg. The European Journal of General Practice. 2007; 13(2): 60-6.
8. Smakowski AL, Hüsing P, Völcker S, Löwe B, Rosmalen JG, Shedden-Mora M, et al. Psychological risk factors of somatic symptom disorder: A systematic review and meta-analysis of cross-sectional and longitudinal studies. Journal of Psychosomatic Research. 2024; 181: 111608.
9. Chauhan A, Jain CK. Psychosomatic disorder: the current implications and challenges. Cardiovascular & Hematological Agents in Medicinal Chemistry. 2024; 22(4): 399-406.
10. Dash S. Psycosomatic disorders an overall review on oral manifestations. Journal of Dentistry and Dental Materials. 2024; 2(1): 1-5.
11. Abdivalyevna AN, Abdukhamid AF. Factors causing personal psychosomatic disorders. International Journal of Advance Scientific Research. 2023; 3(11): 343-7.
12. Philippova A, Malkina O, Korotun V, Shatova E. The role of somatic factors in early childhood and adolescent psychosomatic disorders. Bangladesh Journal of Medical Science. 2023; 22(3): 687-94.
13. Looper KJ, Kirmayer LJ. Hypochondriacal concerns in a community population. Psychological Medicine. 2001; 31(4): 577-84.
14. Yildirim H, Işik K, Aylaz R. The effect of anxiety levels of elderly people in quarantine on depression during covid-19 pandemic. Social Work in Public Health. 2021; 36(2): 194-204.
15. Müller M, Jürgens J, Redaèlli M, Klingberg K, Hautz WE, Stock S. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. 2018; 8(8): 1-10.
16. Grönros J, Nilsson EH, Köteles F, Nordin S. Association between somatic symptoms and modern health worries. Journal of Psychosomatic Research. 2020; 135: 110163.
17. Association AP. The practice of electroconvulsive therapy: recommendations for treatment, training, and privileging (A task force report of the American Psychiatric Association): American Psychiatric Publication; 2024.
18. Fergusson-White CA. Self-regulation in multiple sclerosis: the role of illness cognitions and coping in adjustment [PhD thesis]. Stirling: University of Stirling; 2008.
19. Sauer KS, Witthöft M, Rief W. Somatic symptom disorder and health anxiety: assessment and management. Neurologic Clinics. 2023; 41(4): 745-58.
20. Diamond PR, Dysch L, Daniels J. Health anxiety in stroke survivors: a cross-sectional study on the prevalence of health anxiety in stroke survivors and its impact on quality of life. Disability and Rehabilitation. 2023; 45(1): 27-33.
21. Salkovskis PM, Warwick HM. Morbid preoccupations, health anxiety and reassurance: a cognitive-behavioural approach to hypochondriasis. Behaviour Research and Therapy. 1986; 24(5): 597-602.
22. Windsor NA, Li SH, Joubert A, Upton E, Moulds M, Newby JM. Intrusive thoughts and images in health anxiety: rates, characteristics, and responses. Clinical Psychology & Psychotherapy. 2024; 31(6): 70017.
23. Fink P, Ørnbøl E, Christensen KS. The outcome of health anxiety in primary care. A two-year follow-up study on health care costs and self-rated health. PloS One. 2010; 5(3): 1-12.
24. Mahoney AE, Dobinson K, Millard M, Newby JM. A clinician’s quick guide to evidence-based approaches: health anxiety. Clinical Psychologist. 2024; 1-3.
25. Ghazanfari E, Kazemnejad A, Feizi A, Fesharaki MG, Dinu I, Keshteli AH, et al. The relationship between personality traits and psychosomatic complaints in a sample of Iranian adults. Journal of Affective Disorders. 2020; 261: 253-8.
26. Abdolkarimi M, Sadeghi-Yarandi M, Sakari P. Investigating the relationship between personality traits of hardiness and perfectionism with stress and psychosomatic symptoms: a cross-sectional study among nurses in Iran. BMC Psychology. 2024; 12(1): 1-10.
27. Schmitz N, Hartkamp N, Baldini C, Rollnik J, Tress W. Psychometric properties of the German version of the NEO-FFI in psychosomatic outpatients. Personality and Individual Differences. 2001; 31(5): 713-22.
28. Barlow DH, Ellard KK, Sauer-Zavala S, Bullis JR, Carl JR. The origins of neuroticism. Perspectives on Psychological Science. 2014; 9(5): 481-96.
29. Costa PT, Robert R. Revised NEO personality inventory (NEO PI-R) and NEO five-factor inventory (neo-ffi). Psychological Assessment Resource, 1992.
30. Schultz DP, Schultz SE. Theories of personality. 11th ed. Cengage Learning: Thomson; 2005.
31. Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. The British Journal of Psychiatry. 2005; 186(3): 190-6.
32. Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006; 2(1): 111-33.
33. Weinstock LM, Whisman MA. Neuroticism as a common feature of the depressive and anxiety disorders: a test of the revised integrative hierarchical model in a national sample. Journal of Abnormal Psychology. 2006; 115(1): 68-74.
34. Xia D, Han X, Zeng Y, Wang J, Xu K, Zhang T, et al. Disease trajectory of high neuroticism and the relevance to psychiatric disorders: a retro-prospective cohort study. Acta Psychiatrica Scandinavica. 2024; 149(2): 133-46.
35. Chen YN. The relationship between personality traits, emotional stability and mental health in art vocational and technical college students during epidemic prevention and control. Psychology Research and Behavior Management. 2023; 16: 2857-67.
36. Feist J, Feist GJ, Roberts TA. Theories of personality. 10th ed. Yogyakarta: Pustaka Pelajar; 2008.
37. Smith KE, Mason TB, Lavender JM. Rumination and eating disorder psychopathology: A meta-analysis. Clinical Psychology Review. 2018; 61: 9-23.
38. Li T, Liu T, Han J, Zhang M, Li Z, Zhu Q, et al. The relationship among resilience, rumination and posttraumatic growth in hemodialysis patients in North China. Psychology, Health & Medicine. 2018 Apr 21; 23(4):442-53.
39. Van Natta O. From the Slime and Mud: Rumination as Fuel for Artistic Process [Master thesis]. Florida: University of Central Florida; 2024.
40. Watkins ER, Roberts H. Reflecting on rumination: consequences, causes, mechanisms and treatment of rumination. Behaviour Research and Therapy. 2020; 127: 103573.
41. Seli P, Risko EF, Smilek D, Schacter DL. Mind-wandering with and without intention. Trends in Cognitive Sciences. 2016; 20(8): 605-17.
42. Rickerby N, Krug I, Fuller-Tyszkiewicz M, Forte E, Davenport R, Chayadi E, et al. Rumination across depression, anxiety, and eating disorders in adults: a meta-analytic review. Clinical Psychology: Science and Practice. 2024; 31(2): 25-68.
43. Hwang J, Park S. Gender-specific prevalence and risk factors of sarcopenic obesity in the Korean elderly population: a nationwide cross-sectional study. International Journal of Environmental Research and Public Health. 2023; 20(2): 1-9.
44. Marsa R, Younesi SJ, Barekati S, Ramshini M, Ghyasi H. A Comparative study on stress, anxiety and depression between nursing-home elderly residents and home-dwelling elderly people. Salmand: Iranian Journal of Ageing. 2020; 15(58): 176-87. [Persian]
45. Younis NM, Ibrahim RM, Ahmed MM. Health problems related to quality of life among aging in Iraq. Journal of Current Medical Research and Opinion. 2024; 7(06): 3015-24.
46. Pallant J. SPSS survival manual: A step-by-step guide to data analysis using IBM SPSS. 7th ed. London: Routledge; 2020.
47. Ghasemi E, Zeinab A, Azam N, Ali EM. Prediction of school burnout based on psychosomatic symptoms, personality traits, father-child interaction and its components in students. Rooyesh-e-Ravanshenasi. 2024; 13(6): 191-200. [Persian]
48. Salkovskis PM, Rimes KA, Warwick HM, Clark D. The health anxiety inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine. 2002; 32(5): 843-53.
49. Davoudi I, Nargassi F, Mehrabizadeh M. Gender differences in health anxiety and related dysfunctional beliefs: Controlling for age. Quarterly Journal of Health Psychology. 2012; 1(3): 1-9. [Persian]
50. Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. Journal of Personality and Social Psychology. 1991; 61(1): 115-21.
51. Milani FB, Momeni K, Dehghani-Arani F, Beyramvand Y, Setoudehmaram S, Saffarifard R. The mediating role of rumination in the relationship between high school students with borderline personality disorder and self-injury. Journal of Applied Psycology Research. 2023; 14(1): 85-98. [Persian]
52. Costa PT, McCrae RR. The revised neo personality inventory (NEO-PI-R). In Boyle JG, Matthews G, Saklofske DH, editors. The SAGE handbook of personality theory and assessment. Vol. 2. Personality measurement and testing. Sage Publications, Inc; 2008. p.179-98.
53. Azkhosh M, Asgari A. Five factor model in Iranian culture: A psychometrics analysis of NEO-five factor inventory (NEO-FFI). International Journal of Indian Psychology. 2014; 1(4): 1-24.
54. Lockhart G, MacKinnon DP, Ohlrich V. Mediation analysis in psychosomatic medicine research. Psychosomatic medicine. 2011; 73(1): 29-43.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







