Volume 11, Issue 1 (June 2025)
Elderly Health Journal 2025, 11(1): 22-29 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Roohi G, sabzi Z, Mazraei G, Behnampour N, mancheri H. Effect of Sleep Health Education on the Sleep Quality of Elderly Individuals with Diabetes. Elderly Health Journal 2025; 11 (1) :22-29
URL: http://ehj.ssu.ac.ir/article-1-341-en.html
URL: http://ehj.ssu.ac.ir/article-1-341-en.html
Nursing Research Center, Faculty of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran , zsgorgan@yahoo.com
Full-Text [PDF 624 kb]
(223 Downloads)
| Abstract (HTML) (661 Views)
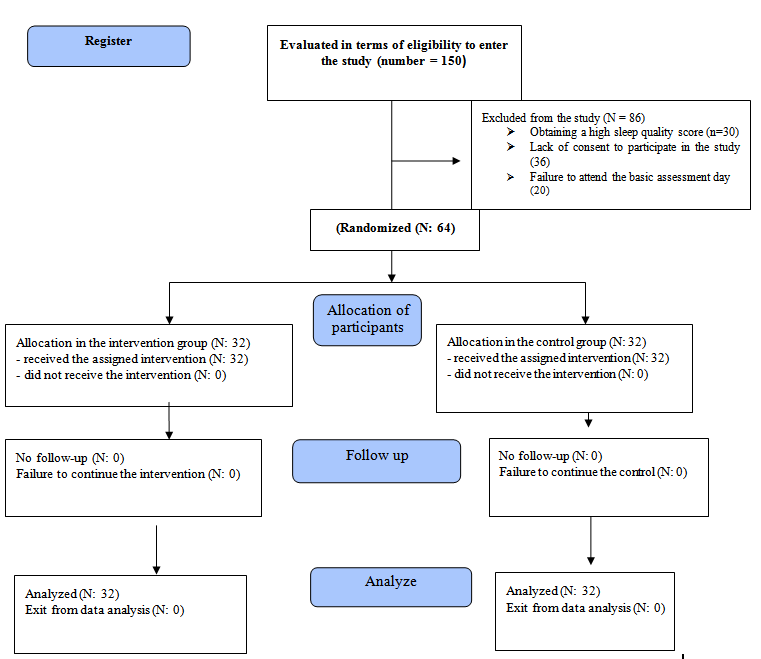
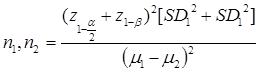
Figure 1. CONSORT process flow
The results of the Friedman test, as presented in Table 3, further demonstrated that within the intervention group, all components of sleep quality, except for "sufficient sleep" and "amount of hypnotic drug use," showed a statistically significant difference across the baseline, one-month, and two-month post-intervention assessments.
Discussion
This study aimed to determine the effect of sleep health education on the sleep quality of elderly individuals with diabetes in Gorgan, Iran. The findings indicate that the mean overall sleep quality score for elderly participants in both the intervention and control groups was low at baseline, suggesting that elderly individuals with diabetes generally experience poor sleep quality at the outset of the study. This aligns with findings from studies by Taheri et al. (13), Hoch et al. (20), Moradi et al. (19), Montazeri Lemrasky et al. (21), and Mottaghi et al. (22), all of which reported similar baseline sleep quality. Furthermore, Fadayevatan et al. (5) conducted a cross-sectional study in Kerman that also reported poor sleep quality among the elderly. Bahrami et al. (23) similarly noted a high prevalence of sleep disorders in the elderly, with 73.5% reporting poor sleep quality. Consistent with these observations, Li et al. (10) found that half of the elderly population in China experienced poor sleep quality.
In this context, it's worth noting that studies consistently show major changes in sleep quality, sleep structure, and circadian rhythm (sleep and wakefulness) with increasing age. The findings of our study, particularly the overall sleep quality score two months after the intervention, indicate that sleep health education was effective in improving the sleep quality of elderly individuals with diabetes. This is supported by a systematic review conducted by Shin et al. (24) in 2016, which suggests that mobile phone-based training can improve sleep quality in various populations.
However, in contrast to our findings, McCrae et al. (25) reported no significant difference in sleep health education outcomes between groups of elderly individuals with and without sleep disorders. A possible reason for this discrepancy could be differences in the individual characteristics and study populations; our study specifically focused on elderly individuals with diabetes.
Within the intervention group, sleep health education, particularly after two months, positively impacted all components of sleep quality except for "medication consumption" and "sleep adequacy." This differs from the findings of Asiri et al. (15), who reported that sleep health education was effective across all components in their intervention group, leading to significant changes both before and after the intervention. This discrepancy might be attributed to differences in the individual characteristics of the research populations, the methods used to deliver the educational program, and the duration of the post-intervention assessment.
References
1. Bagheri-Nesami M, Meskini L, Rostami-ghadi M. The effect of aromatherapy with essential oils of lavender on sleep quality in the elderly. Journal of Gerontology. 2019; 4(3): 63-73. [Persian]
2. Goli Roshan A, Hosseinkhani SN, Norouzadeh R. The relationship between health literacy of elderly diabetics and adherence to treatment, Babol, Iran, 2021. Qom University of Medical Sciences Journal. 2021; 14(12): 70-80. [Persian]
3. Maresova P, Javanmardi E, Barakovic S, Barakovic Husic J, Tomsone S, et al. Consequences of chronic diseases and other limitations associated with old age–a scoping review. BMC Public Health. 2019; 19(1): 1-7.
4. Noohi E, Khandan M, Mirzazadeh A. Effective of electronic education on knowledge attitude and self-care in patient's diabetic type 2 refer to diabetic center of Kerman University of medical science. Iranian Journal of Nursing Research. 2011; 6(22): 73-80. [Persian]
5. Fadayevatan R, Bahrami M, Mohamadzadeh M, Borhaninejad V. Relationship of sleep quality with mental health and blood sugar control in elderly people with diabetes mellitus. Iranian Journal of Ageing. 2020; 14(4): 380-91. [Persian]
6. Hasanpour F, Mehravar F, Badeleh-Shamushaki MT, Mancheri H. The association of health literacy and medication adherence in type 2 diabetic’s patients referring to comprehensive health centers in Gorgan city. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2024; 9(4): 321-33. [Persian]
7. Budhiraja R, Roth T, Hudgel DW, Budhiraja P, Drake CL. Prevalence and polysomnographic correlates of insomnia comorbid with medical disorders. Sleep. 2011; 34(7): 859-67.
8. Alshehri MM, Alkathiry AA, Alenazi AM, Alothman SA, Rucker JL, Phadnis MA, et al. Sleep efficiency and total sleep time in individuals with Type 2 diabetes with and without insomnia symptoms. Sleep Disorders. 2020; 2020(1): 1-12.
9. Tanaka H, Shirakawa S. Sleep health, lifestyle and mental health in the Japanese elderly: ensuring sleep to promote a healthy brain and mind. Journal of Psychosomatic Research. 2004; 56(5): 465-77.
10. Li J, Yao YS, Dong Q, Dong YH, Liu JJ, Yang LS, et al. Characterization and factors associated with sleep quality among rural elderly in China. Archives of Gerontology and Geriatrics. 2013; 56 (1): 237-43.
11. Amini A, Shirvani H, Bazgir B. Effect of rhythmic neural, musculoskeletal exercises on sleep quality in armed forces retirement. Journal of Military Medicine. 2021; 23(2): 10-26. [Persian]
12. Safa A, Adib-Hajbaghery M, Fazel-Darbandi AR. The relationship between sleep quality and quality of life in older adults. Iranian Journal of Psychiatric Nursing. 2015; 3(3): 53-62. [Persian]
13. Taheri Tanjani P, Khodabakhshi H, Etemad K, Mohammadi M. Effect of sleep hygiene education on sleep quality and general health of elderly women with sleep disorders living in Birjand City, Iran, in 2016. Iranian Journal of Ageing. 2019; 14(2): 248-59. [Persian]
14. Torabi A, Ilali ES, Emadian SO, Mousavinasab N. Comparison of the effect of sleep hygiene education with the cognitive and behavioral method on the quality of sleep in elderly. Journal of Gerontology. 2019; 4 (3): 9-17. [Persian]
15. Asiri S, Rahimi H, Kazemnezhad Leyli E, Pourvakhshoori N. The effect of sleep health education based on mobile application on sleep quality of the elderly: a quasi-experimental study. Iranian Journal of Ageing. 2025; 20(1): 136-55. [Persian]
16. Foley DJ, Monjan A, Simonsick EM, Wallace RB, Blazer DG. Incidence and remission of insomnia among elderly adults: an epidemiologic study of 6,800 persons over three years. Sleep. 1999; 22: S366-72.
17. Agargun MY, Kara H, Anlar O. The reliability and validity of Turkish version of Pittsburgh Sleep Quality Index. Turk Psikiyatri Derg. 1996; 7: 107-15.
18. Mirzaei M, Gholamrezaei E, Bidaki R, Fallahzadeh H, Ravaei J. Quality of sleep and methods of management of sleep disorders in elderly of Yazd city in 2016. Journal of Shahid Sadoughi University of Medical Sciences. 2017 Sep 15; 25(6):467-75. [Persian]
19. Moradi M, Mohammadzadeh H, Noori R, Basiri Moghadam K, Sadeghmoghadam L. Effect of a sleep hygiene education program using telephone follow-up method on the sleep quality of the elderly. Iranian Journal of Ageing. 2021; 15(4): 484-95. [Persian]
20. Hoch CC, Reynolds III CF, Buysse DJ, Monk TH, Nowell P, Begley AE, et al. Protecting sleep quality in later life: a pilot study of bed restriction and sleep hygiene. The Journals of Gerontology. 2001; 56(1): 52-9.
21 Montazeri Lemrasky M, Shamsalinia A, Hajiahmadi M, Nasiri M. The effectiveness of education on factors affecting elderly women's sleep. Caspian Journal of Health and Aging. 2018; 3 (1): 59-68. [Persian]
22. Mottaghi R, Kamkar A, Maredpoor A. Effectiveness of cognitive behavior therapy on the quality of sleep in elderly people with insomnia disorder. Iranian Journal of Ageing. 2016; 11(2): 234-43. [Persian]
23 Bahrami M, Dehdashti AR, Karami M. A survey on sleep quality in elderly people living in a nursing home in Damghan city in 2017: A short report. Journal of Rafsanjan University of Medical Sciences. 2017; 16(6): 581-90. [Persian]
24. Shin JC, Kim J, Grigsby-Toussaint D. Mobile phone interventions for sleep disorders and sleep quality: systematic review. JMIR mHealth and UHealth. 2017; 5(9): 7244.
25. McCrae CS, Rowe MA, Dautovich ND, Lichstein KL, Durrence HH, Riedel BW, et al. Sleep hygiene practices in two community dwelling samples of older adults. Sleep. 2006; 29(12): 1551-60.
Full-Text: (267 Views)
Effect of Sleep Health Education on the Sleep Quality of Elderly Individuals with Diabetes
Ghanbar Roohi 1, Zahra Sabzi 1*, Ghazale Mazraei 2, Nasser Behnampour 3, Hamideh Mancheri 1
3. Department of Biostatistics, Faculty of Health, Golestan University of Medical Sciences, Gorgan, Iran
Article history
Received 16 Feb 2025
Accepted 23 Jun 2025
A B S T R A C T
Ghanbar Roohi 1, Zahra Sabzi 1*, Ghazale Mazraei 2, Nasser Behnampour 3, Hamideh Mancheri 1
1. Nursing Research Center, Faculty of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran
2. School of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran3. Department of Biostatistics, Faculty of Health, Golestan University of Medical Sciences, Gorgan, Iran
Article history
Received 16 Feb 2025
Accepted 23 Jun 2025
A B S T R A C T
Introduction: Sleep disorders significantly impact the daily functioning and overall well-being of elderly individuals. Given that non-pharmacological treatments generally yield more sustainable results than medications, this study aimed to evaluate the effectiveness of sleep health education in improving the sleep quality of elderly individuals with diabetes attending a diabetes clinic in Gorgan, Iran.
Methods: This randomized controlled clinical trial was conducted in 2022. A total of 64 eligible elderly patients with diabetes who visited the Gorgan diabetes clinic were randomly assigned to either the intervention or control group. The intervention group received a one-week sleep health education program. Data were collected using the Pittsburgh Sleep Quality Index, administered to both groups at baseline and again one and two months after the intervention. Chi-square and Friedman tests were used to analyze the data using SPSS 21, with a significance level of p < 0.05.
Results: At baseline, the total sleep quality score was 9.66 in the control group and 8.78 in the intervention group. A statistically significant difference in the total sleep quality score was observed only in the intervention group across the three assessment points (baseline, one month, and two months post-intervention) (p < 0.001). In the intervention group, all components of sleep quality, except for sleep adequacy and use of sleep medications, showed a statistically significant difference across the three stages (p < 0.05).
Conclusion: Considering the demonstrated effectiveness of sleep health education on the sleep quality of elderly individuals with diabetes, it is recommended that healthcare personnel prioritize and integrate sleep health education for this population.
Keywords: Sleep Disorder, Aged, Diabetes, Sleep Quality
Methods: This randomized controlled clinical trial was conducted in 2022. A total of 64 eligible elderly patients with diabetes who visited the Gorgan diabetes clinic were randomly assigned to either the intervention or control group. The intervention group received a one-week sleep health education program. Data were collected using the Pittsburgh Sleep Quality Index, administered to both groups at baseline and again one and two months after the intervention. Chi-square and Friedman tests were used to analyze the data using SPSS 21, with a significance level of p < 0.05.
Results: At baseline, the total sleep quality score was 9.66 in the control group and 8.78 in the intervention group. A statistically significant difference in the total sleep quality score was observed only in the intervention group across the three assessment points (baseline, one month, and two months post-intervention) (p < 0.001). In the intervention group, all components of sleep quality, except for sleep adequacy and use of sleep medications, showed a statistically significant difference across the three stages (p < 0.05).
Conclusion: Considering the demonstrated effectiveness of sleep health education on the sleep quality of elderly individuals with diabetes, it is recommended that healthcare personnel prioritize and integrate sleep health education for this population.
Keywords: Sleep Disorder, Aged, Diabetes, Sleep Quality
Copyright © 2025 Elderly Health Journal. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cite.
Introduction
The age structure of the Iranian population has undergone significant shifts over the past 30 to 40 years, indicating a rapidly growing elderly population. Projections suggest that the elderly will constitute 11.3% of the total population by 2025 and a substantial 30% by 2050 (1).
One of the significant challenges faced by the elderly is the development of chronic diseases that can limit their functional abilities (2). Among these, diabetes is particularly noteworthy, requiring diligent self-care due to its complex factors, unpredictable course, and long treatment duration (3). The prevalence of diabetes in the elderly is three times higher than in younger individuals (4).
Diabetes Mellitus (DM) is widely recognized as a common functional impairment in older adults, inherently affecting their physical, mental, and social functioning (5). This disease contributes to a reduced life expectancy and increases the incidence of various complications, including cardiovascular, cerebrovascular, and peripheral vascular diseases, as well as vision, neurological, and renal problems, diabetic foot ulcers, depression, and sleep disturbances (5, 6).
One of the most common issues in diabetic patients is sleep disturbance. Statistics also highlight that sleep problems rank as the third most prevalent complaint among the elderly, following headaches and digestive disorders, and are a frequent reason for their visits to a physician (5). It is well-established that diabetic patients face a higher risk of developing sleep disorders compared to the general population. For instance, the prevalence of insomnia in elderly diabetic individuals is reported to be 25.6%, compared to 21.1% in their non-diabetic counterparts (7).
In individuals with type 2 diabetes, disease symptoms such as hyperglycemia, nocturnal polyuria, hypoglycemia, obesity, pain, and discomfort can contribute to the occurrence of sleep disorders. Recent studies further indicate that diabetes-related symptoms like pain, nervous tension, and depressive symptoms are associated with sleep disturbances (8). Disrupted nighttime sleep can lead to decreased functioning of the hypothalamus, pituitary, and adrenal glands, difficulty concentrating, feelings of fatigue, daytime sleepiness, social maladjustment, depression, and a weakened immune system (9).
Furthermore, sleep disorders can result in restlessness, anxiety, daytime somnolence, reduced mental activity, impaired individual performance, exacerbated cardiovascular complications, diminished quality of life, and increased mortality. Common sleep complaints among the elderly include difficulty initiating sleep, increased sleep latency, nighttime awakenings, early morning awakenings, and daytime sleepiness. Among the various types of sleep-related problems, difficulty falling asleep or staying asleep, and early morning awakening with an inability to fall back asleep are particularly common in older adults (1). One study reported that nearly half (49.7%) of elderly Chinese individuals experienced poor sleep quality (10).
Approaches to improving sleep quality include both pharmacological and non-pharmacological methods. However, the use of medications for sleep disorders in the elderly can lead to adverse outcomes such as drug interactions (due to polypharmacy), an increased risk of falls, and a loss of functional ability (5). In contrast, while the effectiveness of non-pharmacological treatments may be slower than that of sleeping pills, they offer more durable results and do not carry side effects like addiction. Therefore, identifying non-pharmacological alternatives for improving sleep quality in the elderly is crucial (11).
Studies have demonstrated that various interventions, such as aromatherapy, massage, hot showers, and proper nutrition, are effective in enhancing sleep quality (12). While many factors influencing sleep cannot be directly modified or controlled, thereby making them difficult targets for interventions, sleep health is one modifiable aspect. The fundamental approach to treating any type of sleep disorder often involves sleep health education. Sleep health education is a component of behavioral therapy, with the primary goal of behavioral techniques used in insomnia treatment being to modify behaviors that exacerbate sleep disorders. Sleep health itself refers to taking steps to support the natural rhythm of sleep and wakefulness and to promote restful sleep (13). Beyond healthy individuals, a sleep health program can also benefit those experiencing mild to moderate insomnia without obvious physical problems (14). In this regard, Asiri et al. conducted a study to determine the effect of mobile phone application-based sleep health education on sleep quality in elderly individuals covered by the State Pension Fund of Rasht. Their study results showed that sleep health education had a statistically significant positive effect on sleep quality in all domains except sleep efficiency (P < 0.05) (15).
Therefore, considering the high prevalence of sleep disorders in the elderly, their adverse consequences, and the limited research in this specific area, the present study was designed and implemented. Its aim is to investigate the effect of sleep health education on improving sleep quality in elderly individuals with diabetes who referred to a diabetes clinic in 2022.
Method
Study design
The current study is a randomized controlled clinical trial conducted in 2022.
Participants
The research population for this study included individuals referring to Deziani Specialized Clinic in Gorgan with a diagnosis of DM.
Inclusion criteria for participation were:
One of the significant challenges faced by the elderly is the development of chronic diseases that can limit their functional abilities (2). Among these, diabetes is particularly noteworthy, requiring diligent self-care due to its complex factors, unpredictable course, and long treatment duration (3). The prevalence of diabetes in the elderly is three times higher than in younger individuals (4).
Diabetes Mellitus (DM) is widely recognized as a common functional impairment in older adults, inherently affecting their physical, mental, and social functioning (5). This disease contributes to a reduced life expectancy and increases the incidence of various complications, including cardiovascular, cerebrovascular, and peripheral vascular diseases, as well as vision, neurological, and renal problems, diabetic foot ulcers, depression, and sleep disturbances (5, 6).
One of the most common issues in diabetic patients is sleep disturbance. Statistics also highlight that sleep problems rank as the third most prevalent complaint among the elderly, following headaches and digestive disorders, and are a frequent reason for their visits to a physician (5). It is well-established that diabetic patients face a higher risk of developing sleep disorders compared to the general population. For instance, the prevalence of insomnia in elderly diabetic individuals is reported to be 25.6%, compared to 21.1% in their non-diabetic counterparts (7).
In individuals with type 2 diabetes, disease symptoms such as hyperglycemia, nocturnal polyuria, hypoglycemia, obesity, pain, and discomfort can contribute to the occurrence of sleep disorders. Recent studies further indicate that diabetes-related symptoms like pain, nervous tension, and depressive symptoms are associated with sleep disturbances (8). Disrupted nighttime sleep can lead to decreased functioning of the hypothalamus, pituitary, and adrenal glands, difficulty concentrating, feelings of fatigue, daytime sleepiness, social maladjustment, depression, and a weakened immune system (9).
Furthermore, sleep disorders can result in restlessness, anxiety, daytime somnolence, reduced mental activity, impaired individual performance, exacerbated cardiovascular complications, diminished quality of life, and increased mortality. Common sleep complaints among the elderly include difficulty initiating sleep, increased sleep latency, nighttime awakenings, early morning awakenings, and daytime sleepiness. Among the various types of sleep-related problems, difficulty falling asleep or staying asleep, and early morning awakening with an inability to fall back asleep are particularly common in older adults (1). One study reported that nearly half (49.7%) of elderly Chinese individuals experienced poor sleep quality (10).
Approaches to improving sleep quality include both pharmacological and non-pharmacological methods. However, the use of medications for sleep disorders in the elderly can lead to adverse outcomes such as drug interactions (due to polypharmacy), an increased risk of falls, and a loss of functional ability (5). In contrast, while the effectiveness of non-pharmacological treatments may be slower than that of sleeping pills, they offer more durable results and do not carry side effects like addiction. Therefore, identifying non-pharmacological alternatives for improving sleep quality in the elderly is crucial (11).
Studies have demonstrated that various interventions, such as aromatherapy, massage, hot showers, and proper nutrition, are effective in enhancing sleep quality (12). While many factors influencing sleep cannot be directly modified or controlled, thereby making them difficult targets for interventions, sleep health is one modifiable aspect. The fundamental approach to treating any type of sleep disorder often involves sleep health education. Sleep health education is a component of behavioral therapy, with the primary goal of behavioral techniques used in insomnia treatment being to modify behaviors that exacerbate sleep disorders. Sleep health itself refers to taking steps to support the natural rhythm of sleep and wakefulness and to promote restful sleep (13). Beyond healthy individuals, a sleep health program can also benefit those experiencing mild to moderate insomnia without obvious physical problems (14). In this regard, Asiri et al. conducted a study to determine the effect of mobile phone application-based sleep health education on sleep quality in elderly individuals covered by the State Pension Fund of Rasht. Their study results showed that sleep health education had a statistically significant positive effect on sleep quality in all domains except sleep efficiency (P < 0.05) (15).
Therefore, considering the high prevalence of sleep disorders in the elderly, their adverse consequences, and the limited research in this specific area, the present study was designed and implemented. Its aim is to investigate the effect of sleep health education on improving sleep quality in elderly individuals with diabetes who referred to a diabetes clinic in 2022.
Method
Study design
The current study is a randomized controlled clinical trial conducted in 2022.
Participants
The research population for this study included individuals referring to Deziani Specialized Clinic in Gorgan with a diagnosis of DM.
Inclusion criteria for participation were:
- Age over 65 years.
- Literacy (ability to read and write).
- Ability to communicate.
- Diagnosis of DM (specifically referring to Deziani Specialized Clinic in Gorgan, with at least one year passed since their diagnosis, a history of drug treatment, and an active file in the clinic).
- No known progressive chronic diseases (such as cancer and lupus, confirmed through file review).
- A score of 6 or higher on the Pittsburgh Sleep Quality Index (PSQI) (16).
- Willingness to participate in the study.
- No psychological problems, based on self-report and healthcare documentation at the center.
Exclusion criteria included:
- Death of the elderly participant during the study.
- Failure to participate in more than one training session.
- Relocation of the elderly participant.
- Illness requiring hospitalization and non-attendance at sessions.
- Withdrawal of the patient from continued study participation.
Instrumentation
Data collection utilized a two-part questionnaire. The first part gathered demographic information (including age, sex, marital status, number of children, etc.). The second part consisted of the standard PSQI.
The PSQI, developed in 1989 by Buysse et al. at the University of Pittsburgh Medical Center, assesses sleep disturbances over the past month. This questionnaire comprises 18 questions across seven components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each component is scored from zero (no problem) to three (very serious problem). The scores from all seven components are then summed to yield a total score, ranging from 0 to 21. A higher score in any component or in the overall score indicates poorer sleep quality. Scores of 0, 1, 2, and 3 on each scale indicate normal conditions, mild, moderate, and severe problems, respectively. A total score of 6 or more signifies poor sleep quality. The original developers reported an internal reliability (Cronbach's alpha) of 0.83 for the questionnaire (16, 17). For the Iranian version of this questionnaire, a validity of 0.88 and a reliability of 0.70 were obtained (18).
Data collection
After obtaining permission from the ethics committee and research council, data collection commenced. Given the reported prevalence of sleep disorders in the elderly (67%) (19), an initial 150 elderly individuals with DM who met the inclusion criteria were conveniently selected. First, necessary arrangements were made for these individuals to attend the Deziani Clinic Diabetes Center via telephone. Upon arrival, the researcher introduced themselves, explained the study objectives, obtained verbal consent, and provided them with the sleep quality questionnaire, which they completed in the researcher's presence. After questionnaire completion and calculation of their sleep quality scores, those with moderate to poor sleep quality scores (64 individuals) were randomly assigned to either the control group (32 individuals) or the intervention group (32 individuals) using a block randomization method. (Figure 1)
Data collection utilized a two-part questionnaire. The first part gathered demographic information (including age, sex, marital status, number of children, etc.). The second part consisted of the standard PSQI.
The PSQI, developed in 1989 by Buysse et al. at the University of Pittsburgh Medical Center, assesses sleep disturbances over the past month. This questionnaire comprises 18 questions across seven components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each component is scored from zero (no problem) to three (very serious problem). The scores from all seven components are then summed to yield a total score, ranging from 0 to 21. A higher score in any component or in the overall score indicates poorer sleep quality. Scores of 0, 1, 2, and 3 on each scale indicate normal conditions, mild, moderate, and severe problems, respectively. A total score of 6 or more signifies poor sleep quality. The original developers reported an internal reliability (Cronbach's alpha) of 0.83 for the questionnaire (16, 17). For the Iranian version of this questionnaire, a validity of 0.88 and a reliability of 0.70 were obtained (18).
Data collection
After obtaining permission from the ethics committee and research council, data collection commenced. Given the reported prevalence of sleep disorders in the elderly (67%) (19), an initial 150 elderly individuals with DM who met the inclusion criteria were conveniently selected. First, necessary arrangements were made for these individuals to attend the Deziani Clinic Diabetes Center via telephone. Upon arrival, the researcher introduced themselves, explained the study objectives, obtained verbal consent, and provided them with the sleep quality questionnaire, which they completed in the researcher's presence. After questionnaire completion and calculation of their sleep quality scores, those with moderate to poor sleep quality scores (64 individuals) were randomly assigned to either the control group (32 individuals) or the intervention group (32 individuals) using a block randomization method. (Figure 1)
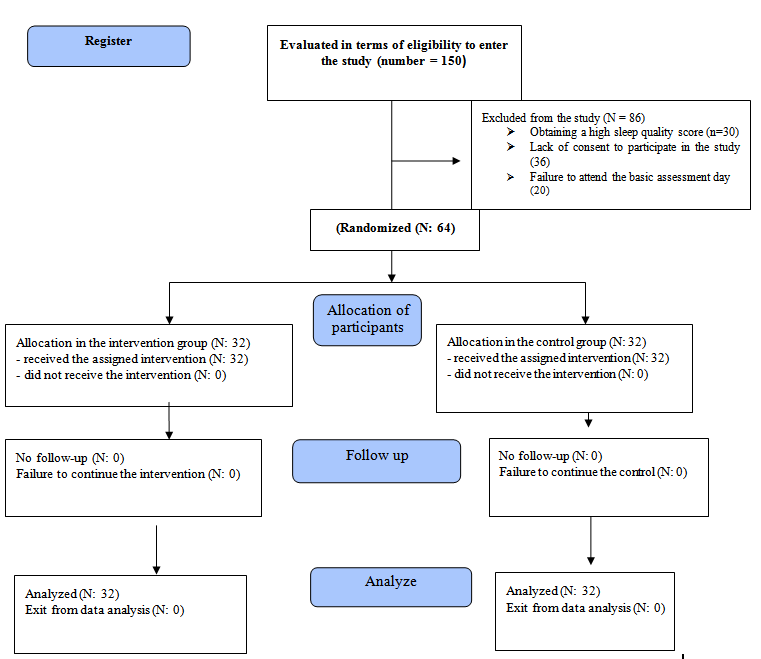
Figure 1. CONSORT process flow
Sample size
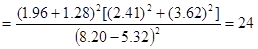
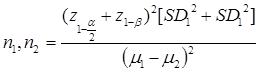
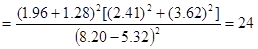
The sample size was calculated based on the mean and standard deviation of data from a study by Moradi et al. (10) and the results presented in Table 3. With a 95% confidence level and 90% power (meaning α = 0.05 and β = 0.10), the initial calculation using the following formula determined a requirement of 24 participants per group. Accounting for a 25% dropout rate, the final sample size was set at 32 individuals per group (19).
Sample size formula:
Intervention group
For elderly individuals with DM in the intervention group, a sleep health education program was implemented in addition to their usual care. This program consisted of three consecutive weekly sessions for each group. A total of 32 participants were divided into four groups of 8 people.
The education sessions were held in the morning in one of the classrooms at the Deziani Diabetes Center, with each session lasting 45 minutes. These sessions were conducted in person by a master's degree student in geriatric nursing, under the supervision of faculty advisors, using a lecture and question-and-answer method. It's important to note that due to the conditions of the COVID-19 pandemic, educational groups were kept smaller with strict adherence to health protocols.
The educational content covered the importance of sleep in the lives of the elderly, age-related changes in sleep, and a comprehensive sleep health program (including nutrition, physical activity, sleep environment, and sleep schedule adjustment) (19). Additionally, each participant in the intervention group received a sleep health education booklet in pamphlet form during the final training session. The summary of these educational sessions is presented in Table 1.
The PSQI was administered to both the intervention and control groups at one and two months after the completion of the educational program.
To ensure proper attendance and completion of the PSQI for the intervention groups one and two months after the intervention, the researcher scheduled their follow-up visits based on their group assignments and the completion time of their educational program. A few days before the appointed time, the researcher would re-confirm the time and location for completing the questionnaires via phone contact to maximize participation.
Control group
For elderly individuals with DM in the control group, eligible participants who met the inclusion criteria received only the standard, routine care provided by the clinic. One and two months after the study began, these diabetic elderly individuals were invited to complete the PSQI. Given that there were 32 people in the control group, to ensure accurate questionnaire completion and facilitate their presence, this process was managed within a maximum period of one week. A few days prior to their scheduled date, they received a phone call confirming the time (referral between 8 AM and 12 PM) and the clinic's location, requesting their attendance to complete the questionnaire again. At the conclusion of the study, the educational booklet was also provided to the control group.
Statistical analysis
Quantitative variables were described by reporting their mean and standard deviation, while qualitative variables were presented using frequency distribution tables. To compare the means of quantitative variables, the Shapiro-Wilk test was first used to check for normality of data distribution. Depending on the normality of the data distribution, the Friedman test, Chi-square test, and Mann-Whitney U test were employed. Data were entered into Excel and then imported and analyzed using R software version 3.5.1. The significance level for all tests was set at p < 0.05.
Ethical considerations
This study adhered to the ethical framework of the Declaration of Helsinki. Permission was obtained from the Ethics Committee of Golestan University of Medical Sciences, Gorgan, Iran (ethical code IR.GOUMS.REC.1401.066), and the study was registered with the Iranian Registry of Clinical Trials (IRCT20220411054493N1, Registration date: 2022-07-30). All participants were informed of the voluntary nature of their participation and were assured of their freedom to withdraw from the study at any time. We also ensured the confidentiality of participants' personal information. Furthermore, written informed consent was obtained from each participant.
Results
Regarding gender, participants in the intervention group were 65.6% women and 34.4% men. In the control group, 44.9% were women and 55.1% were men. In terms of education level, the majority of participants in both the intervention group (62.5%) and the control group (59.4%) had less than a high school diploma. The Chi-square test revealed no statistically significant difference between the control and intervention groups concerning gender (p = 0.131), education level (p=0.964), or job status (p=0.914).
Friedman's test revealed a statistically significant difference in the total sleep quality score in the intervention group across the three time points (before intervention, one month, and two months later) (p < 0.001). In contrast, the control group did not show a statistically significant difference in total sleep quality over the same period (p=0.088). (Figure 2)
Friedman's statistical test also indicated that the mean rank total sleep quality score did not differ significantly between the intervention and control groups at baseline (p = 0.071) or one month post-intervention (p = 0.136). However, two months after the intervention, a significant difference emerged (p < 0.001), with the total sleep quality score in the intervention group showing a significant decrease. (Table 2)
The sample size was calculated based on the mean and standard deviation of data from a study by Moradi et al. (10) and the results presented in Table 3. With a 95% confidence level and 90% power (meaning α = 0.05 and β = 0.10), the initial calculation using the following formula determined a requirement of 24 participants per group. Accounting for a 25% dropout rate, the final sample size was set at 32 individuals per group (19).
Sample size formula:
Intervention group
For elderly individuals with DM in the intervention group, a sleep health education program was implemented in addition to their usual care. This program consisted of three consecutive weekly sessions for each group. A total of 32 participants were divided into four groups of 8 people.
The education sessions were held in the morning in one of the classrooms at the Deziani Diabetes Center, with each session lasting 45 minutes. These sessions were conducted in person by a master's degree student in geriatric nursing, under the supervision of faculty advisors, using a lecture and question-and-answer method. It's important to note that due to the conditions of the COVID-19 pandemic, educational groups were kept smaller with strict adherence to health protocols.
The educational content covered the importance of sleep in the lives of the elderly, age-related changes in sleep, and a comprehensive sleep health program (including nutrition, physical activity, sleep environment, and sleep schedule adjustment) (19). Additionally, each participant in the intervention group received a sleep health education booklet in pamphlet form during the final training session. The summary of these educational sessions is presented in Table 1.
The PSQI was administered to both the intervention and control groups at one and two months after the completion of the educational program.
To ensure proper attendance and completion of the PSQI for the intervention groups one and two months after the intervention, the researcher scheduled their follow-up visits based on their group assignments and the completion time of their educational program. A few days before the appointed time, the researcher would re-confirm the time and location for completing the questionnaires via phone contact to maximize participation.
Control group
For elderly individuals with DM in the control group, eligible participants who met the inclusion criteria received only the standard, routine care provided by the clinic. One and two months after the study began, these diabetic elderly individuals were invited to complete the PSQI. Given that there were 32 people in the control group, to ensure accurate questionnaire completion and facilitate their presence, this process was managed within a maximum period of one week. A few days prior to their scheduled date, they received a phone call confirming the time (referral between 8 AM and 12 PM) and the clinic's location, requesting their attendance to complete the questionnaire again. At the conclusion of the study, the educational booklet was also provided to the control group.
Statistical analysis
Quantitative variables were described by reporting their mean and standard deviation, while qualitative variables were presented using frequency distribution tables. To compare the means of quantitative variables, the Shapiro-Wilk test was first used to check for normality of data distribution. Depending on the normality of the data distribution, the Friedman test, Chi-square test, and Mann-Whitney U test were employed. Data were entered into Excel and then imported and analyzed using R software version 3.5.1. The significance level for all tests was set at p < 0.05.
Ethical considerations
This study adhered to the ethical framework of the Declaration of Helsinki. Permission was obtained from the Ethics Committee of Golestan University of Medical Sciences, Gorgan, Iran (ethical code IR.GOUMS.REC.1401.066), and the study was registered with the Iranian Registry of Clinical Trials (IRCT20220411054493N1, Registration date: 2022-07-30). All participants were informed of the voluntary nature of their participation and were assured of their freedom to withdraw from the study at any time. We also ensured the confidentiality of participants' personal information. Furthermore, written informed consent was obtained from each participant.
Results
Regarding gender, participants in the intervention group were 65.6% women and 34.4% men. In the control group, 44.9% were women and 55.1% were men. In terms of education level, the majority of participants in both the intervention group (62.5%) and the control group (59.4%) had less than a high school diploma. The Chi-square test revealed no statistically significant difference between the control and intervention groups concerning gender (p = 0.131), education level (p=0.964), or job status (p=0.914).
Friedman's test revealed a statistically significant difference in the total sleep quality score in the intervention group across the three time points (before intervention, one month, and two months later) (p < 0.001). In contrast, the control group did not show a statistically significant difference in total sleep quality over the same period (p=0.088). (Figure 2)
Friedman's statistical test also indicated that the mean rank total sleep quality score did not differ significantly between the intervention and control groups at baseline (p = 0.071) or one month post-intervention (p = 0.136). However, two months after the intervention, a significant difference emerged (p < 0.001), with the total sleep quality score in the intervention group showing a significant decrease. (Table 2)
Table1. Sleep health education program for the elderly
.png)
Figure2. Comparison of the average overall sleep quality score at three study times in the two intervention and control groups
Table 2. Comparison of the total sleep mean rank score in the three investigated times between the two control and intervention groups
| Nicotine, alcohol and caffeine are found in energy drinks, coffee, tea, soft drinks, chocolate and some painkillers. Smoking before going to sleep decreases the quality of sleep by reducing the duration of deep sleep, increasing nighttime restlessness and fragmenting sleep. Hunger or overeating before going to sleep also causes bad sleep. It is recommended to eat a light meal before going to bed. The quality of sleep can be increased by reducing the consumption of liquids before sleep due to the possible need to use the toilet between sleeps. |
Nutrition |
| Do not do mental and physical exercises close to bedtime. Do relaxing exercises before bedtime. |
Activity |
| The sleeping environment should be cool, calm and very dark. Inappropriate temperature, light and noise disturb sleep. Choose a suitable and comfortable mattress, pillow and bed. Remove the clock from the side of the bed and keep it out of sight. |
Sleeping environment |
| Consider a specific time to sleep and stick to it. Limit daytime naps: Napping during the day reduces the quality of sleep at night. However, a short nap can help improve mood, alertness and daily performance. You can take a 20-30 minute nap every day. |
Set a fixed sleep schedule |
| Some colors induce relaxation and improve sleep, including blue and green. You can use these colors for the bedroom. If you can't fall asleep within 20 minutes, get out of bed, go to another room and go back to bed again. |
Suitable bedroom design |
.png)
Figure2. Comparison of the average overall sleep quality score at three study times in the two intervention and control groups
Table 2. Comparison of the total sleep mean rank score in the three investigated times between the two control and intervention groups
| p | Intervention group | Control group | |
| 0.071 | 2.42 | 2.13 | Before intervention |
| 0.136 | 2.48 | 2.06 | One month after the intervention |
| 0.0001>* | 1.09 | 1.81 | Two months after the intervention |
The results of the Friedman test, as presented in Table 3, further demonstrated that within the intervention group, all components of sleep quality, except for "sufficient sleep" and "amount of hypnotic drug use," showed a statistically significant difference across the baseline, one-month, and two-month post-intervention assessments.
Discussion
This study aimed to determine the effect of sleep health education on the sleep quality of elderly individuals with diabetes in Gorgan, Iran. The findings indicate that the mean overall sleep quality score for elderly participants in both the intervention and control groups was low at baseline, suggesting that elderly individuals with diabetes generally experience poor sleep quality at the outset of the study. This aligns with findings from studies by Taheri et al. (13), Hoch et al. (20), Moradi et al. (19), Montazeri Lemrasky et al. (21), and Mottaghi et al. (22), all of which reported similar baseline sleep quality. Furthermore, Fadayevatan et al. (5) conducted a cross-sectional study in Kerman that also reported poor sleep quality among the elderly. Bahrami et al. (23) similarly noted a high prevalence of sleep disorders in the elderly, with 73.5% reporting poor sleep quality. Consistent with these observations, Li et al. (10) found that half of the elderly population in China experienced poor sleep quality.
In this context, it's worth noting that studies consistently show major changes in sleep quality, sleep structure, and circadian rhythm (sleep and wakefulness) with increasing age. The findings of our study, particularly the overall sleep quality score two months after the intervention, indicate that sleep health education was effective in improving the sleep quality of elderly individuals with diabetes. This is supported by a systematic review conducted by Shin et al. (24) in 2016, which suggests that mobile phone-based training can improve sleep quality in various populations.
However, in contrast to our findings, McCrae et al. (25) reported no significant difference in sleep health education outcomes between groups of elderly individuals with and without sleep disorders. A possible reason for this discrepancy could be differences in the individual characteristics and study populations; our study specifically focused on elderly individuals with diabetes.
Within the intervention group, sleep health education, particularly after two months, positively impacted all components of sleep quality except for "medication consumption" and "sleep adequacy." This differs from the findings of Asiri et al. (15), who reported that sleep health education was effective across all components in their intervention group, leading to significant changes both before and after the intervention. This discrepancy might be attributed to differences in the individual characteristics of the research populations, the methods used to deliver the educational program, and the duration of the post-intervention assessment.
Table 3. Comparison of sleep quality components in three stages: before, 1 and 2 months intervention
| Components of sleep quality | Time |
Mean rank score control group |
p |
Mean rank score intervention group |
p |
| A person's overall description of sleep quality | Before | 2.08 | 0.222 |
2.41 | > 0.001 |
| One month after | 1.94 | 2.41 | |||
| Two months after | 1.98 | 1.19 | |||
| Delay in falling asleep | Before | 2.00 | 0.177 |
2.13 | > 0.001 |
| One month after | 2.09 | 2.23 | |||
| Two months after | 1.91 | 1.64 | |||
| Useful sleep duration | Before | 2.09 | 0.177 | 2.16 | > 0.001 |
| One month after | 2.00 | 2.16 | |||
| Two months after | 1.91 | 1.69 | |||
| Sufficient sleep |
Before | 2.05 | 0.778 | 2.03 | 0.556 |
| One month after | 1.95 | 2.03 | |||
| Two months after | 2.00 | 1.94 | |||
| Sleep disorders | Before | 2.00 | 0.815 | 2.17 | > 0.001 |
| One month after | 2.05 | 2.17 | |||
| Two months after | 1.95 | 1.66 | |||
| Amount of hypnotic drug used | Before | 2.00 | 1.00 | 2.00 | 1.00 |
| One month after | 2.00 | 2.00 | |||
| Two months after | 2.00 | 2.00 | |||
| Morning performance | Before | 2.00 | 1.00 |
2.23 | > 0.001 |
| One month after | 2.00 | 2.23 | |||
| Two months after | 2.00 | 1.53 |
Conclusion
Considering that the sleep health education program significantly improved the sleep quality of elderly individuals with diabetes two months after the intervention, we recommend that this sleep education program be incorporated into the training of healthcare employees, particularly nurses, within health and treatment centers. This would equip them to effectively enhance the sleep quality of elderly patients with diabetes.
Study limitations
The age and physical conditions of the study participants presented a limitation within the intervention group, requiring the researcher to dedicate more time to material presentation and to provide clearer, more thorough explanations of the educational content. Another limitation of the current research involved the mental and psychological conditions of the participants while answering questionnaire questions, which may have influenced their post-test scores. This, however, was beyond the researcher's control.
Consent of interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgments
This study is derived from a Master's thesis conducted at the Gorgan School of Nursing and Midwifery. The researchers extend their sincere appreciation to the Research Center, the Vice President of Research and Technology of Gorgan University of Medical Sciences, the staff of the medical centers, and the invaluable elderly participants who contributed to this research.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Funding
This article was extracted from a research project approved by the Nursing Research Committee, Golestan University of Medical Sciences.
Authors’ contributions
All authors contributed to the writing of the article and approved the final version of the manuscript.
Considering that the sleep health education program significantly improved the sleep quality of elderly individuals with diabetes two months after the intervention, we recommend that this sleep education program be incorporated into the training of healthcare employees, particularly nurses, within health and treatment centers. This would equip them to effectively enhance the sleep quality of elderly patients with diabetes.
Study limitations
The age and physical conditions of the study participants presented a limitation within the intervention group, requiring the researcher to dedicate more time to material presentation and to provide clearer, more thorough explanations of the educational content. Another limitation of the current research involved the mental and psychological conditions of the participants while answering questionnaire questions, which may have influenced their post-test scores. This, however, was beyond the researcher's control.
Consent of interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgments
This study is derived from a Master's thesis conducted at the Gorgan School of Nursing and Midwifery. The researchers extend their sincere appreciation to the Research Center, the Vice President of Research and Technology of Gorgan University of Medical Sciences, the staff of the medical centers, and the invaluable elderly participants who contributed to this research.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Funding
This article was extracted from a research project approved by the Nursing Research Committee, Golestan University of Medical Sciences.
Authors’ contributions
All authors contributed to the writing of the article and approved the final version of the manuscript.
- GHM: Conceptualization, study design, and data acquisition.
- GhR: Conceptualization, study design, data acquisition, data interpretation, and approval of the submitted version.
- ZS: Conceptualization, study design, data acquisition, data interpretation, and approval of the submitted version.
- NB: Study design, data analysis, and approval of the submitted version.
- HM: Conceptualization, study design, data acquisition, data interpretation, and approval of the submitted version.
References
1. Bagheri-Nesami M, Meskini L, Rostami-ghadi M. The effect of aromatherapy with essential oils of lavender on sleep quality in the elderly. Journal of Gerontology. 2019; 4(3): 63-73. [Persian]
2. Goli Roshan A, Hosseinkhani SN, Norouzadeh R. The relationship between health literacy of elderly diabetics and adherence to treatment, Babol, Iran, 2021. Qom University of Medical Sciences Journal. 2021; 14(12): 70-80. [Persian]
3. Maresova P, Javanmardi E, Barakovic S, Barakovic Husic J, Tomsone S, et al. Consequences of chronic diseases and other limitations associated with old age–a scoping review. BMC Public Health. 2019; 19(1): 1-7.
4. Noohi E, Khandan M, Mirzazadeh A. Effective of electronic education on knowledge attitude and self-care in patient's diabetic type 2 refer to diabetic center of Kerman University of medical science. Iranian Journal of Nursing Research. 2011; 6(22): 73-80. [Persian]
5. Fadayevatan R, Bahrami M, Mohamadzadeh M, Borhaninejad V. Relationship of sleep quality with mental health and blood sugar control in elderly people with diabetes mellitus. Iranian Journal of Ageing. 2020; 14(4): 380-91. [Persian]
6. Hasanpour F, Mehravar F, Badeleh-Shamushaki MT, Mancheri H. The association of health literacy and medication adherence in type 2 diabetic’s patients referring to comprehensive health centers in Gorgan city. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2024; 9(4): 321-33. [Persian]
7. Budhiraja R, Roth T, Hudgel DW, Budhiraja P, Drake CL. Prevalence and polysomnographic correlates of insomnia comorbid with medical disorders. Sleep. 2011; 34(7): 859-67.
8. Alshehri MM, Alkathiry AA, Alenazi AM, Alothman SA, Rucker JL, Phadnis MA, et al. Sleep efficiency and total sleep time in individuals with Type 2 diabetes with and without insomnia symptoms. Sleep Disorders. 2020; 2020(1): 1-12.
9. Tanaka H, Shirakawa S. Sleep health, lifestyle and mental health in the Japanese elderly: ensuring sleep to promote a healthy brain and mind. Journal of Psychosomatic Research. 2004; 56(5): 465-77.
10. Li J, Yao YS, Dong Q, Dong YH, Liu JJ, Yang LS, et al. Characterization and factors associated with sleep quality among rural elderly in China. Archives of Gerontology and Geriatrics. 2013; 56 (1): 237-43.
11. Amini A, Shirvani H, Bazgir B. Effect of rhythmic neural, musculoskeletal exercises on sleep quality in armed forces retirement. Journal of Military Medicine. 2021; 23(2): 10-26. [Persian]
12. Safa A, Adib-Hajbaghery M, Fazel-Darbandi AR. The relationship between sleep quality and quality of life in older adults. Iranian Journal of Psychiatric Nursing. 2015; 3(3): 53-62. [Persian]
13. Taheri Tanjani P, Khodabakhshi H, Etemad K, Mohammadi M. Effect of sleep hygiene education on sleep quality and general health of elderly women with sleep disorders living in Birjand City, Iran, in 2016. Iranian Journal of Ageing. 2019; 14(2): 248-59. [Persian]
14. Torabi A, Ilali ES, Emadian SO, Mousavinasab N. Comparison of the effect of sleep hygiene education with the cognitive and behavioral method on the quality of sleep in elderly. Journal of Gerontology. 2019; 4 (3): 9-17. [Persian]
15. Asiri S, Rahimi H, Kazemnezhad Leyli E, Pourvakhshoori N. The effect of sleep health education based on mobile application on sleep quality of the elderly: a quasi-experimental study. Iranian Journal of Ageing. 2025; 20(1): 136-55. [Persian]
16. Foley DJ, Monjan A, Simonsick EM, Wallace RB, Blazer DG. Incidence and remission of insomnia among elderly adults: an epidemiologic study of 6,800 persons over three years. Sleep. 1999; 22: S366-72.
17. Agargun MY, Kara H, Anlar O. The reliability and validity of Turkish version of Pittsburgh Sleep Quality Index. Turk Psikiyatri Derg. 1996; 7: 107-15.
18. Mirzaei M, Gholamrezaei E, Bidaki R, Fallahzadeh H, Ravaei J. Quality of sleep and methods of management of sleep disorders in elderly of Yazd city in 2016. Journal of Shahid Sadoughi University of Medical Sciences. 2017 Sep 15; 25(6):467-75. [Persian]
19. Moradi M, Mohammadzadeh H, Noori R, Basiri Moghadam K, Sadeghmoghadam L. Effect of a sleep hygiene education program using telephone follow-up method on the sleep quality of the elderly. Iranian Journal of Ageing. 2021; 15(4): 484-95. [Persian]
20. Hoch CC, Reynolds III CF, Buysse DJ, Monk TH, Nowell P, Begley AE, et al. Protecting sleep quality in later life: a pilot study of bed restriction and sleep hygiene. The Journals of Gerontology. 2001; 56(1): 52-9.
21 Montazeri Lemrasky M, Shamsalinia A, Hajiahmadi M, Nasiri M. The effectiveness of education on factors affecting elderly women's sleep. Caspian Journal of Health and Aging. 2018; 3 (1): 59-68. [Persian]
22. Mottaghi R, Kamkar A, Maredpoor A. Effectiveness of cognitive behavior therapy on the quality of sleep in elderly people with insomnia disorder. Iranian Journal of Ageing. 2016; 11(2): 234-43. [Persian]
23 Bahrami M, Dehdashti AR, Karami M. A survey on sleep quality in elderly people living in a nursing home in Damghan city in 2017: A short report. Journal of Rafsanjan University of Medical Sciences. 2017; 16(6): 581-90. [Persian]
24. Shin JC, Kim J, Grigsby-Toussaint D. Mobile phone interventions for sleep disorders and sleep quality: systematic review. JMIR mHealth and UHealth. 2017; 5(9): 7244.
25. McCrae CS, Rowe MA, Dautovich ND, Lichstein KL, Durrence HH, Riedel BW, et al. Sleep hygiene practices in two community dwelling samples of older adults. Sleep. 2006; 29(12): 1551-60.
Type of Study: Research |
Subject:
Special
Received: 2025/02/16 | Accepted: 2025/06/23 | Published: 2025/06/20
Received: 2025/02/16 | Accepted: 2025/06/23 | Published: 2025/06/20
References
1. Bagheri-Nesami M, Meskini L, Rostami-ghadi M. The effect of aromatherapy with essential oils of lavender on sleep quality in the elderly. Journal of Gerontology. 2019; 4(3): 63-73. [Persian]
2. Goli Roshan A, Hosseinkhani SN, Norouzadeh R. The relationship between health literacy of elderly diabetics and adherence to treatment, Babol, Iran, 2021. Qom University of Medical Sciences Journal. 2021; 14(12): 70-80. [Persian]
3. Maresova P, Javanmardi E, Barakovic S, Barakovic Husic J, Tomsone S, et al. Consequences of chronic diseases and other limitations associated with old age–a scoping review. BMC Public Health. 2019; 19(1): 1-7.
4. Noohi E, Khandan M, Mirzazadeh A. Effective of electronic education on knowledge attitude and self-care in patient's diabetic type 2 refer to diabetic center of Kerman University of medical science. Iranian Journal of Nursing Research. 2011; 6(22): 73-80. [Persian]
5. Fadayevatan R, Bahrami M, Mohamadzadeh M, Borhaninejad V. Relationship of sleep quality with mental health and blood sugar control in elderly people with diabetes mellitus. Iranian Journal of Ageing. 2020; 14(4): 380-91. [Persian]
6. Hasanpour F, Mehravar F, Badeleh-Shamushaki MT, Mancheri H. The association of health literacy and medication adherence in type 2 diabetic’s patients referring to comprehensive health centers in Gorgan city. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2024; 9(4): 321-33. [Persian]
7. Budhiraja R, Roth T, Hudgel DW, Budhiraja P, Drake CL. Prevalence and polysomnographic correlates of insomnia comorbid with medical disorders. Sleep. 2011; 34(7): 859-67.
8. Alshehri MM, Alkathiry AA, Alenazi AM, Alothman SA, Rucker JL, Phadnis MA, et al. Sleep efficiency and total sleep time in individuals with Type 2 diabetes with and without insomnia symptoms. Sleep Disorders. 2020; 2020(1): 1-12.
9. Tanaka H, Shirakawa S. Sleep health, lifestyle and mental health in the Japanese elderly: ensuring sleep to promote a healthy brain and mind. Journal of Psychosomatic Research. 2004; 56(5): 465-77.
10. Li J, Yao YS, Dong Q, Dong YH, Liu JJ, Yang LS, et al. Characterization and factors associated with sleep quality among rural elderly in China. Archives of Gerontology and Geriatrics. 2013; 56 (1): 237-43.
11. Amini A, Shirvani H, Bazgir B. Effect of rhythmic neural, musculoskeletal exercises on sleep quality in armed forces retirement. Journal of Military Medicine. 2021; 23(2): 10-26. [Persian]
12. Safa A, Adib-Hajbaghery M, Fazel-Darbandi AR. The relationship between sleep quality and quality of life in older adults. Iranian Journal of Psychiatric Nursing. 2015; 3(3): 53-62. [Persian]
13. Taheri Tanjani P, Khodabakhshi H, Etemad K, Mohammadi M. Effect of sleep hygiene education on sleep quality and general health of elderly women with sleep disorders living in Birjand City, Iran, in 2016. Iranian Journal of Ageing. 2019; 14(2): 248-59. [Persian]
14. Torabi A, Ilali ES, Emadian SO, Mousavinasab N. Comparison of the effect of sleep hygiene education with the cognitive and behavioral method on the quality of sleep in elderly. Journal of Gerontology. 2019; 4 (3): 9-17. [Persian]
15. Asiri S, Rahimi H, Kazemnezhad Leyli E, Pourvakhshoori N. The effect of sleep health education based on mobile application on sleep quality of the elderly: a quasi-experimental study. Iranian Journal of Ageing. 2025; 20(1): 136-55. [Persian]
16. Foley DJ, Monjan A, Simonsick EM, Wallace RB, Blazer DG. Incidence and remission of insomnia among elderly adults: an epidemiologic study of 6,800 persons over three years. Sleep. 1999; 22: S366-72.
17. Agargun MY, Kara H, Anlar O. The reliability and validity of Turkish version of Pittsburgh Sleep Quality Index. Turk Psikiyatri Derg. 1996; 7: 107-15.
18. Mirzaei M, Gholamrezaei E, Bidaki R, Fallahzadeh H, Ravaei J. Quality of sleep and methods of management of sleep disorders in elderly of Yazd city in 2016. Journal of Shahid Sadoughi University of Medical Sciences. 2017 Sep 15; 25(6):467-75. [Persian]
19. Moradi M, Mohammadzadeh H, Noori R, Basiri Moghadam K, Sadeghmoghadam L. Effect of a sleep hygiene education program using telephone follow-up method on the sleep quality of the elderly. Iranian Journal of Ageing. 2021; 15(4): 484-95. [Persian]
20. Hoch CC, Reynolds III CF, Buysse DJ, Monk TH, Nowell P, Begley AE, et al. Protecting sleep quality in later life: a pilot study of bed restriction and sleep hygiene. The Journals of Gerontology. 2001; 56(1): 52-9.
21. Montazeri Lemrasky M, Shamsalinia A, Hajiahmadi M, Nasiri M. The effectiveness of education on factors affecting elderly women's sleep. Caspian Journal of Health and Aging. 2018; 3 (1): 59-68. [Persian]
22. Mottaghi R, Kamkar A, Maredpoor A. Effectiveness of cognitive behavior therapy on the quality of sleep in elderly people with insomnia disorder. Iranian Journal of Ageing. 2016; 11(2): 234-43. [Persian]
23. Bahrami M, Dehdashti AR, Karami M. A survey on sleep quality in elderly people living in a nursing home in Damghan city in 2017: A short report. Journal of Rafsanjan University of Medical Sciences. 2017; 16(6): 581-90. [Persian]
24. Shin JC, Kim J, Grigsby-Toussaint D. Mobile phone interventions for sleep disorders and sleep quality: systematic review. JMIR mHealth and UHealth. 2017; 5(9): 7244.
25. McCrae CS, Rowe MA, Dautovich ND, Lichstein KL, Durrence HH, Riedel BW, et al. Sleep hygiene practices in two community dwelling samples of older adults. Sleep. 2006; 29(12): 1551-60.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |