Volume 10, Issue 1 (June 2024)
Elderly Health Journal 2024, 10(1): 70-75 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghorbanalipour M, Alilou S, Babalou K, Akbarlou N. Depression, Perfectionism, and Hypertension in the Elderly: A Path Analysis Examining Worry, Ambiguity Tolerance, and Problem-Solving. Elderly Health Journal 2024; 10 (1) :70-75
URL: http://ehj.ssu.ac.ir/article-1-318-en.html
URL: http://ehj.ssu.ac.ir/article-1-318-en.html
Department of Psychology, Faculty of Humanities, Azad University of Urmia, Khoy, Urmia, Iran , Masoudqorbanalipour@gmail.com
Full-Text [PDF 646 kb]
(300 Downloads)
| Abstract (HTML) (919 Views)
Table 1. Descriptive indicators of demographic data of the studied sample
Table 2. Correlations matrix for depression, perfectionism, hypertension, worry, ambiguity tolerance and problem-solving
Table 3. Multivariate regression- prediction of hypertension with depression, perfectionism, worry, ambiguity tolerance and problem-solving
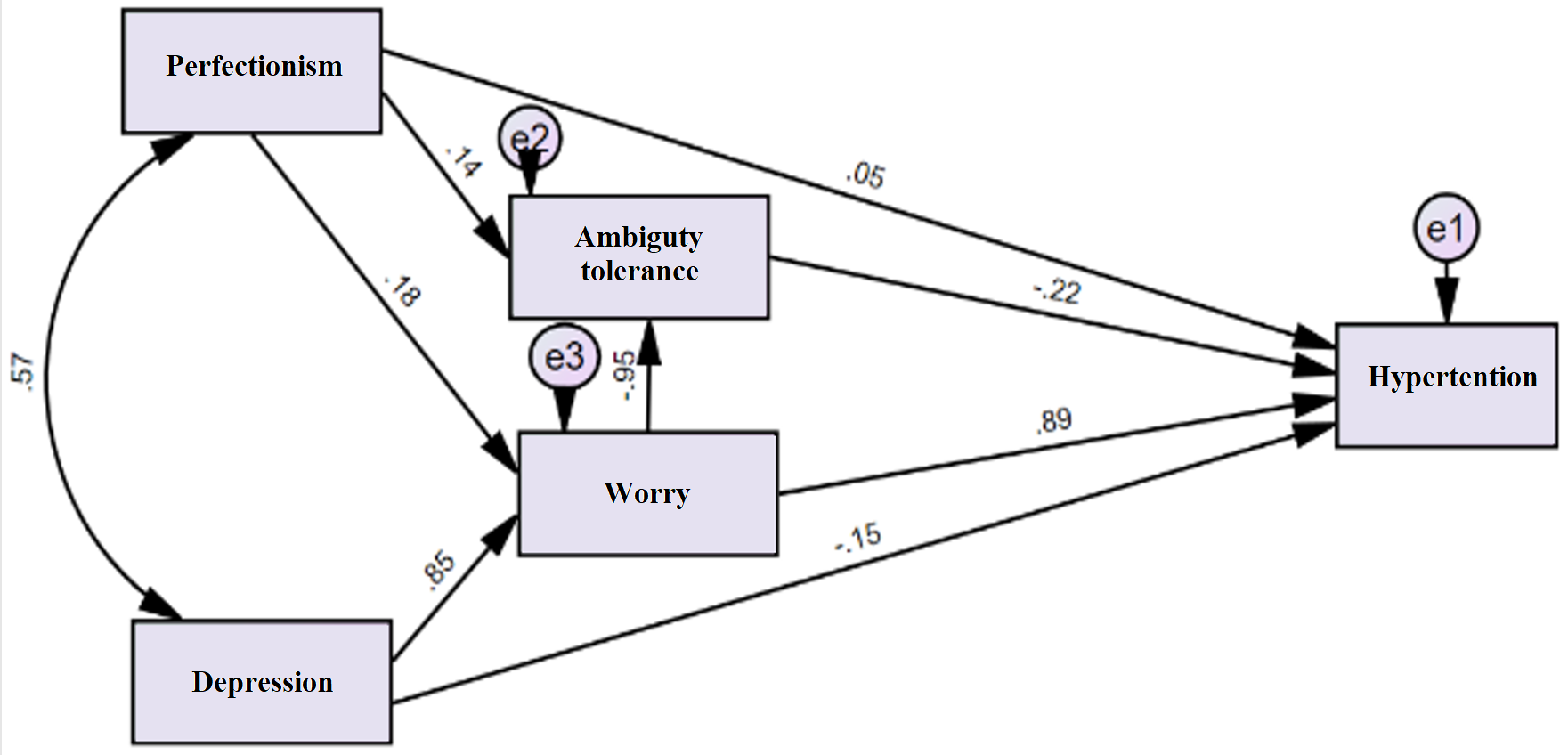
Figure 1. Path analysis model with standard coefficients for depression, perfectionism, hypertension, worry, ambiguity tolerance and problem-solving
Full-Text: (470 Views)
Depression, Perfectionism, and Hypertension in the Elderly: A Path Analysis Examining Worry, Ambiguity Tolerance, and Problem-Solving
Masood Ghorbanalipour 1*, Shahla Alilou 2, Kosar Babalou 1, Nika Akbarlou 3
Received 11 May 2024
Accepted 22 Jun 2024
A B S T R A C T
Introduction: Hypertension is a prevalent condition among the elderly, significantly contributing to the burden of cardiovascular disease and related complications. This study examined how depression and perfectionism influence hypertension in older adults. It also explored how worry, tolerance for ambiguity, and problem-solving skills might influence this relationship.
Methods: Researchers recruited 192 participants with hypertension from a health center in Khoy city, Urmia, Iran. Participants completed questionnaires that assessed depression, perfectionism, worry, ambiguity tolerance, and problem-solving skills. Statistical methods were used to analyze the data and identify relationships between these factors and hypertension.
Results: Depression, perfectionism, worry, and ambiguity tolerance were all significantly associated with hypertension. Interestingly, problem-solving skills were not linked to blood pressure. Further analysis revealed that worry played a reinforcing role in the link between depression/perfectionism and hypertension, while ambiguity tolerance had a protective effect. In other words, higher worry levels strengthened the association between depression/perfectionism and high blood pressure, while greater tolerance for ambiguity lessened this association.
Conclusion: These findings suggest that emotional factors like worry and intolerance for ambiguity can significantly impact blood pressure in older adults. Therefore, managing these emotions alongside depression and perfectionistic tendencies may be crucial for controlling hypertension.
Keywords: Hypertension, Worry, Depression, Perfectionism, Ambiguity Tolerance
Copyright © 2024 Elderly Health Journal. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cite.
Masood Ghorbanalipour 1*, Shahla Alilou 2, Kosar Babalou 1, Nika Akbarlou 3
- Department of Psychology, Faculty of Humanities, Azad University of Urmia, Khoy Branch, Khoy, Iran
- Department of Psychology, Faculty of Humanities, Shahid Madani University of Azerbaijan, Tabriz, Iran
- Department of Psychology, Faculty of Medicine, Azad University of Urmia, Urmia, Iran
Received 11 May 2024
Accepted 22 Jun 2024
A B S T R A C T
Introduction: Hypertension is a prevalent condition among the elderly, significantly contributing to the burden of cardiovascular disease and related complications. This study examined how depression and perfectionism influence hypertension in older adults. It also explored how worry, tolerance for ambiguity, and problem-solving skills might influence this relationship.
Methods: Researchers recruited 192 participants with hypertension from a health center in Khoy city, Urmia, Iran. Participants completed questionnaires that assessed depression, perfectionism, worry, ambiguity tolerance, and problem-solving skills. Statistical methods were used to analyze the data and identify relationships between these factors and hypertension.
Results: Depression, perfectionism, worry, and ambiguity tolerance were all significantly associated with hypertension. Interestingly, problem-solving skills were not linked to blood pressure. Further analysis revealed that worry played a reinforcing role in the link between depression/perfectionism and hypertension, while ambiguity tolerance had a protective effect. In other words, higher worry levels strengthened the association between depression/perfectionism and high blood pressure, while greater tolerance for ambiguity lessened this association.
Conclusion: These findings suggest that emotional factors like worry and intolerance for ambiguity can significantly impact blood pressure in older adults. Therefore, managing these emotions alongside depression and perfectionistic tendencies may be crucial for controlling hypertension.
Keywords: Hypertension, Worry, Depression, Perfectionism, Ambiguity Tolerance
Copyright © 2024 Elderly Health Journal. This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/) which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cite.
Introduction
High blood pressure is a common and serious health concern for older adults, significantly impacting their well-being and quality of life (1, 2). As the population ages globally, understanding the link between psychological factors and hypertension in this group becomes increasingly important (3). This is particularly relevant in Iran, where hypertension is rising and poses a significant physical, financial, and emotional burden (4).
Depression, characterized by persistent sadness, hopelessness, and loss of interest, may contribute to developing and worsening hypertension (5). Older adults often face challenges like loss, declining health, and social isolation, which can trigger or worsen depression (6, 7). Interestingly, research suggests a connection between lower depression scores and lower blood pressure in younger adults, even considering lifestyle factors (8).
Perfectionism, a personality trait characterized by setting extremely high standards, self-criticism, and a fear of mistakes, may also play a role in hypertension (9). The constant pressure to meet unrealistic expectations and the fear of failure associated with perfectionism can contribute to chronic stress and negative emotions, potentially impacting blood pressure regulation (10). Studies have shown that individuals with higher standards tend to have more stable systolic blood pressure (the upper pressure reading), while those with lower standards may experience declines. Similarly, higher self-critical perfectionism is linked to sustained diastolic blood pressure (the lower reading), whereas lower self-criticism is associated with decreases (11).
Beyond depression and perfectionism, emotional factors like worry and tolerance for ambiguity might also influence blood pressure. Excessive worry can lead to chronic stress responses and increase blood pressure (12). Conversely, the ability to tolerate uncertain or ambiguous situations (ambiguity tolerance) might be protective. Individuals with low tolerance may experience higher stress and physiological arousal, contributing to hypertension (13). Problem-solving skills, encompassing the ability to effectively manage challenges, may also influence the relationship between psychological factors and blood pressure by reducing stress and emotional distress (14).
This study employs a path analysis approach to explore these complex relationships in older adults. Path analysis allows us to examine both direct and indirect effects, providing a more comprehensive picture of the underlying mechanisms (15). By examining how depression and perfectionism might contribute to hypertension in the elderly, and the potential mediating role of worry, ambiguity tolerance, and problem-solving ability, we aim to gain insights into the psychological factors influencing blood pressure in this population.
Understanding the role of these psychological factors has significant implications for preventing and treating hypertension in older adults. By identifying the specific mechanisms at play, healthcare professionals can develop targeted strategies to reduce the risk and manage hypertension more effectively. Interventions addressing depression, perfectionism, worry, ambiguity tolerance, and problem-solving skills may hold promise for improving blood pressure regulation and overall cardiovascular health in older adults.
Furthermore, this study contributes to the growing body of research on the psychological aspects of hypertension, particularly in elderly populations. By investigating the specific pathways through which these variables interact, we expand our understanding of the complex interplay between psychological factors and blood pressure. It also highlights the importance of considering multiple psychological factors simultaneously, as they may interact and have cumulative effects on blood pressure regulation.
Methods
Study design and participants
This study employed a descriptive correlational design. The target population included all individuals with hypertension who visited the Motahari and Samadzadeh Health Center in Khoy city, Urmia, Iran during 2023.
To determine the sample size, we used the Green's formula (N ≥ 8M + 50). This formula considers the number of predictor variables (M) in the study (16, 17). Based on this formula, the minimum recommended sample size for correlation studies is at least 90. To ensure greater certainty, we recruited 192 participants. Participants were selected using a convenience sampling method. The only inclusion criterion was being over 60 years old.
Measures
Beck Depression Inventory (BDI): This 21-question self-report questionnaire assesses the severity of depression symptoms. It has a high ability to distinguish between normal and depressed individuals (18). Scores range from 0 to 63, with higher scores indicating greater depression severity. Scores are interpreted as follows:
0-13: No depression
14-19: Mild depression
20-28: Moderate depression
29: +Severe depression
The BDI has demonstrated good reliability and validity in both the original English version and the Farsi translation used in this study (18-20).
Penn State Worry Questionnaire (PSWQ): Developed in 1990, the PSWQ is a 16-item self-assessment tool used to measure general worry tendency. Scores range from 0 to 64, with higher scores indicating greater worry. The PSWQ has established reliability and validity in both English and Farsi (21).
Problem-Solving Inventory (PSI): This 35-item questionnaire assesses how individuals perceive and approach their problems (22). Scores range from 0 to 175, with higher scores indicating more adaptive problem-solving skills. The PSI has shown good reliability and validity in previous research (22- 24).
McLean Ambiguity Tolerance Questionnaire: This 22-item questionnaire measures an individual's tolerance for uncertainty or ambiguity (25). Scores range from 22 to 110, with higher scores indicating greater ambiguity tolerance. The McLean Ambiguity Tolerance Questionnaire has demonstrated good reliability and validity in both English and Farsi (25- 27).
Tehran Multidimensional Perfectionism Scale (TMPS): This 30-item questionnaire assesses three dimensions of perfectionism: self-oriented, other-oriented, and community-oriented (28). Scores range from 10 to 50 for each subscale, with higher scores indicating stronger perfectionist tendencies in that domain. The TMPS has shown good reliability and validity in the Farsi language (28).
Blood pressure measurement tool
Littmann class 2 stethoscope and Riester sphygmomanometer were used to measure blood pressure. In order to measure the blood pressure, the nurse measured the blood pressure on two occasions with a time interval of approximately 5 minutes with the mentioned instruments and the average of these two blood pressures was recorded.
Statistical analysis
Data analysis was performed using SPSS-24 software for initial analyses and AMOS-26 software for path analysis. Before conducting statistical tests, the data was screened for missing values and outliers. No missing data points were identified. Univariate outliers, assessed using boxplots, were corrected by considering values outside the range of one standard deviation from the mean. Multivariate outliers were analyzed using Mahala Nobis distances, and none were identified based on the criteria outlined by Mears, et al (29).
Pearson's correlation coefficients were calculated to assess the relationships between the study variables. Multivariate regression analysis was conducted to predict blood pressure. Path analysis was used to examine the hypothesized relationships between the variables and their influence on blood pressure.
Ethical considerations
This study adhered to ethical principles including confidentiality and informed consent. The study protocol was reviewed and approved by the Ethics Committee of Islamic Azad University, Urmia Branch (ethics identifier: IR.IAU.URMIA.REC.1402.091).
Results
The sample consisted of 192 participants, with 45 (23.2%) being single and 147 (76.8%) married. There were 112 women (57.7%) and 80 men (42.3%). The average age of the participants was 64 years old (standard deviation = 3 years). (Table 1)
All correlations were statistically significant (p < 0.05), as shown in table 2. Ambiguity tolerance had the strongest negative correlation with blood pressure (r = -0.88), while problem-solving had the weakest negative correlation with perfectionism (r = -0.26).
Results indicated that problem-solving was not a significant predictor of blood pressure. (Table 3) Therefore, problem-solving was excluded from further analysis in the path model.
The results of path analysis showed a good model fit, with the RMSEA index below 0.05 and GFI, CFI, NFI, and IFI indices all exceeding 0.90. These findings suggest that the proposed model adequately explains the data. Perfectionism directly and indirectly (through its influence on ambiguity tolerance and worry) predicts hypertension. Depression directly and indirectly (through its influence on ambiguity tolerance and worry) predicts hypertension.
Worry and ambiguity tolerance are significant predictors of hypertension, with worry influencing blood pressure through ambiguity tolerance. Figure 1 visually depicts the path model with standardized coefficients.
Depression, characterized by persistent sadness, hopelessness, and loss of interest, may contribute to developing and worsening hypertension (5). Older adults often face challenges like loss, declining health, and social isolation, which can trigger or worsen depression (6, 7). Interestingly, research suggests a connection between lower depression scores and lower blood pressure in younger adults, even considering lifestyle factors (8).
Perfectionism, a personality trait characterized by setting extremely high standards, self-criticism, and a fear of mistakes, may also play a role in hypertension (9). The constant pressure to meet unrealistic expectations and the fear of failure associated with perfectionism can contribute to chronic stress and negative emotions, potentially impacting blood pressure regulation (10). Studies have shown that individuals with higher standards tend to have more stable systolic blood pressure (the upper pressure reading), while those with lower standards may experience declines. Similarly, higher self-critical perfectionism is linked to sustained diastolic blood pressure (the lower reading), whereas lower self-criticism is associated with decreases (11).
Beyond depression and perfectionism, emotional factors like worry and tolerance for ambiguity might also influence blood pressure. Excessive worry can lead to chronic stress responses and increase blood pressure (12). Conversely, the ability to tolerate uncertain or ambiguous situations (ambiguity tolerance) might be protective. Individuals with low tolerance may experience higher stress and physiological arousal, contributing to hypertension (13). Problem-solving skills, encompassing the ability to effectively manage challenges, may also influence the relationship between psychological factors and blood pressure by reducing stress and emotional distress (14).
This study employs a path analysis approach to explore these complex relationships in older adults. Path analysis allows us to examine both direct and indirect effects, providing a more comprehensive picture of the underlying mechanisms (15). By examining how depression and perfectionism might contribute to hypertension in the elderly, and the potential mediating role of worry, ambiguity tolerance, and problem-solving ability, we aim to gain insights into the psychological factors influencing blood pressure in this population.
Understanding the role of these psychological factors has significant implications for preventing and treating hypertension in older adults. By identifying the specific mechanisms at play, healthcare professionals can develop targeted strategies to reduce the risk and manage hypertension more effectively. Interventions addressing depression, perfectionism, worry, ambiguity tolerance, and problem-solving skills may hold promise for improving blood pressure regulation and overall cardiovascular health in older adults.
Furthermore, this study contributes to the growing body of research on the psychological aspects of hypertension, particularly in elderly populations. By investigating the specific pathways through which these variables interact, we expand our understanding of the complex interplay between psychological factors and blood pressure. It also highlights the importance of considering multiple psychological factors simultaneously, as they may interact and have cumulative effects on blood pressure regulation.
Methods
Study design and participants
This study employed a descriptive correlational design. The target population included all individuals with hypertension who visited the Motahari and Samadzadeh Health Center in Khoy city, Urmia, Iran during 2023.
To determine the sample size, we used the Green's formula (N ≥ 8M + 50). This formula considers the number of predictor variables (M) in the study (16, 17). Based on this formula, the minimum recommended sample size for correlation studies is at least 90. To ensure greater certainty, we recruited 192 participants. Participants were selected using a convenience sampling method. The only inclusion criterion was being over 60 years old.
Measures
Beck Depression Inventory (BDI): This 21-question self-report questionnaire assesses the severity of depression symptoms. It has a high ability to distinguish between normal and depressed individuals (18). Scores range from 0 to 63, with higher scores indicating greater depression severity. Scores are interpreted as follows:
0-13: No depression
14-19: Mild depression
20-28: Moderate depression
29: +Severe depression
The BDI has demonstrated good reliability and validity in both the original English version and the Farsi translation used in this study (18-20).
Penn State Worry Questionnaire (PSWQ): Developed in 1990, the PSWQ is a 16-item self-assessment tool used to measure general worry tendency. Scores range from 0 to 64, with higher scores indicating greater worry. The PSWQ has established reliability and validity in both English and Farsi (21).
Problem-Solving Inventory (PSI): This 35-item questionnaire assesses how individuals perceive and approach their problems (22). Scores range from 0 to 175, with higher scores indicating more adaptive problem-solving skills. The PSI has shown good reliability and validity in previous research (22- 24).
McLean Ambiguity Tolerance Questionnaire: This 22-item questionnaire measures an individual's tolerance for uncertainty or ambiguity (25). Scores range from 22 to 110, with higher scores indicating greater ambiguity tolerance. The McLean Ambiguity Tolerance Questionnaire has demonstrated good reliability and validity in both English and Farsi (25- 27).
Tehran Multidimensional Perfectionism Scale (TMPS): This 30-item questionnaire assesses three dimensions of perfectionism: self-oriented, other-oriented, and community-oriented (28). Scores range from 10 to 50 for each subscale, with higher scores indicating stronger perfectionist tendencies in that domain. The TMPS has shown good reliability and validity in the Farsi language (28).
Blood pressure measurement tool
Littmann class 2 stethoscope and Riester sphygmomanometer were used to measure blood pressure. In order to measure the blood pressure, the nurse measured the blood pressure on two occasions with a time interval of approximately 5 minutes with the mentioned instruments and the average of these two blood pressures was recorded.
Statistical analysis
Data analysis was performed using SPSS-24 software for initial analyses and AMOS-26 software for path analysis. Before conducting statistical tests, the data was screened for missing values and outliers. No missing data points were identified. Univariate outliers, assessed using boxplots, were corrected by considering values outside the range of one standard deviation from the mean. Multivariate outliers were analyzed using Mahala Nobis distances, and none were identified based on the criteria outlined by Mears, et al (29).
Pearson's correlation coefficients were calculated to assess the relationships between the study variables. Multivariate regression analysis was conducted to predict blood pressure. Path analysis was used to examine the hypothesized relationships between the variables and their influence on blood pressure.
Ethical considerations
This study adhered to ethical principles including confidentiality and informed consent. The study protocol was reviewed and approved by the Ethics Committee of Islamic Azad University, Urmia Branch (ethics identifier: IR.IAU.URMIA.REC.1402.091).
Results
The sample consisted of 192 participants, with 45 (23.2%) being single and 147 (76.8%) married. There were 112 women (57.7%) and 80 men (42.3%). The average age of the participants was 64 years old (standard deviation = 3 years). (Table 1)
All correlations were statistically significant (p < 0.05), as shown in table 2. Ambiguity tolerance had the strongest negative correlation with blood pressure (r = -0.88), while problem-solving had the weakest negative correlation with perfectionism (r = -0.26).
Results indicated that problem-solving was not a significant predictor of blood pressure. (Table 3) Therefore, problem-solving was excluded from further analysis in the path model.
The results of path analysis showed a good model fit, with the RMSEA index below 0.05 and GFI, CFI, NFI, and IFI indices all exceeding 0.90. These findings suggest that the proposed model adequately explains the data. Perfectionism directly and indirectly (through its influence on ambiguity tolerance and worry) predicts hypertension. Depression directly and indirectly (through its influence on ambiguity tolerance and worry) predicts hypertension.
Worry and ambiguity tolerance are significant predictors of hypertension, with worry influencing blood pressure through ambiguity tolerance. Figure 1 visually depicts the path model with standardized coefficients.
Table 1. Descriptive indicators of demographic data of the studied sample
| Variables | Frequency (Mean) | Percent (St D.) | |
| Marriage | Married | 149 | 76.8% |
| Single | 45 | 23.2% | |
| Gender | Male | 82 | 42.3% |
| Female | 112 | 57.7% | |
| Blood Pressure | Systolic | (145.7 mm-Hg) | (± 4.5) |
| Diastolic | (93.2 mm-Hg) | (± 5.2) | |
Table 2. Correlations matrix for depression, perfectionism, hypertension, worry, ambiguity tolerance and problem-solving
| Variables | Blood pressure | Perfectionism | Ambiguity tolerance | Worry | Depression |
| Perfectionism | 0.659** | ||||
| Ambiguity tolerance | -0.887** | -0.482** | |||
| Worry | 0.895** | 0.384** | -0.854** | ||
| Depression | 0.486** | 0.589** | -0.624** | 0.754** | |
| Problem-solving | -0.345** | -0.264* | 0.412** | -0.477** | -0.417** |
Table 3. Multivariate regression- prediction of hypertension with depression, perfectionism, worry, ambiguity tolerance and problem-solving
| Independent variables | Dependent variable. | B | Standard Beta | T | p | R | R2 |
| Perfectionism | Blood pressure | 0.01 | 0.04 | 2.46 | 0.015 | 0.98 | 0.96 |
| Ambiguity tolerance | -0.06 | -0.22 | -7.98 | 0.001 | |||
| Worry | 0.40 | 0.89 | 15.13 | 0.001 | |||
| Depression | -0.07 | -0.14 | -3.15 | 0.002 | |||
| Problem-solving | 0.00 | 0.01 | 0.71 | 0.474 |
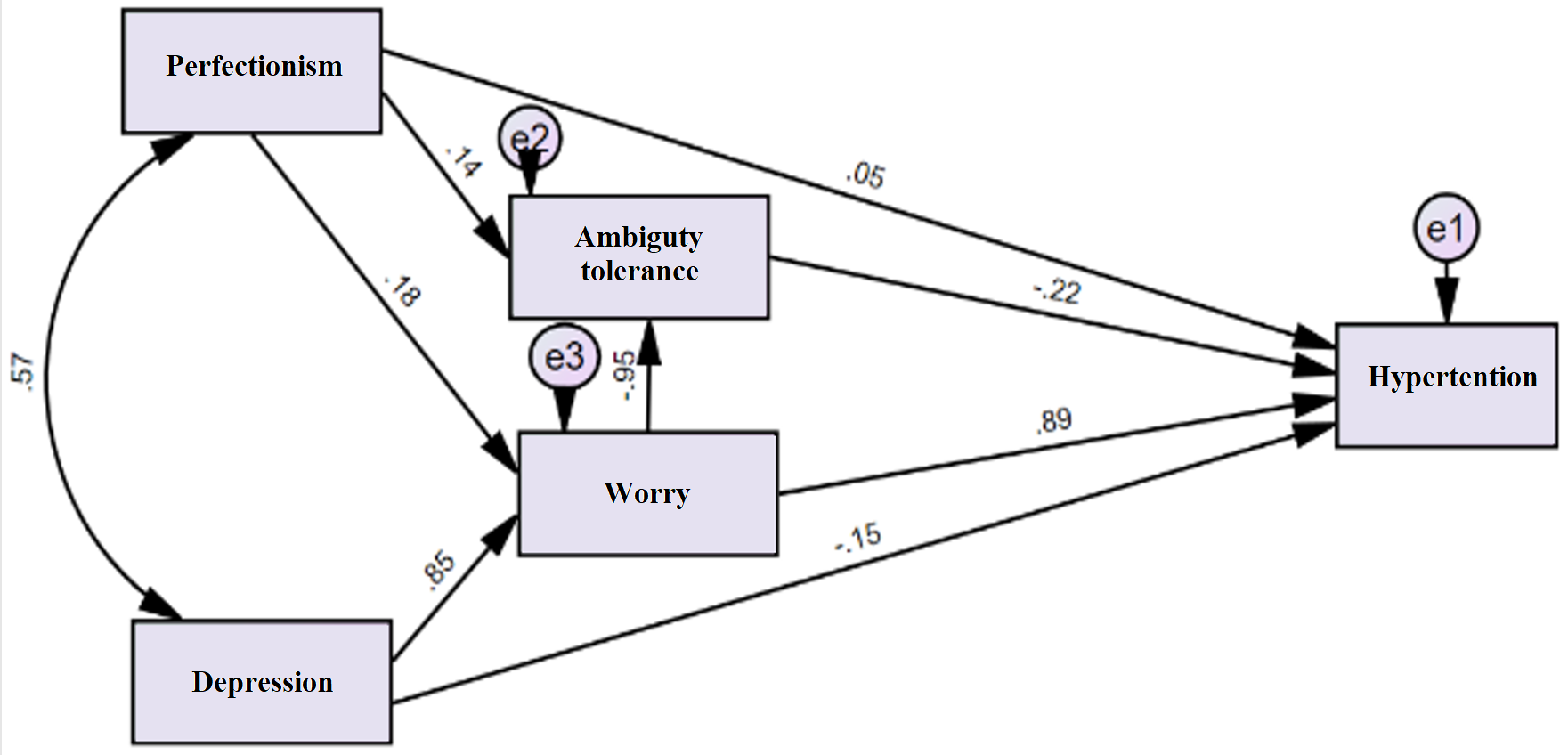
Figure 1. Path analysis model with standard coefficients for depression, perfectionism, hypertension, worry, ambiguity tolerance and problem-solving
Discussion
This study investigated the role of emotional factors (worry, depression), personality traits (perfectionism), and problem-solving abilities in predicting hypertension in older adults, considering the potential mediating effects of ambiguity tolerance. Our findings revealed that problem-solving ability was not a significant predictor of blood pressure and was therefore excluded from further analyses. However, worry, depression, ambiguity tolerance, and perfectionism all played significant roles in hypertension.
These results align with previous research by Albert et al., (11) and Bhat et al., (8). Bhat et al., found an inverse relationship between depression and anxiety scores with hypertension in young adults, partially consistent with our findings for depression but not anxiety. In contrast, our study showed a positive association between worry and hypertension. Additionally, our findings support Albert et al.'s observation that high levels of perfectionistic self-criticism are linked to elevated blood pressure.
The significant role of perfectionism in hypertension can be explained by the constant stress and pressure associated with striving for unrealistic standards. This stress can directly elevate blood pressure. Perfectionism also has an indirect effect through its influence on ambiguity tolerance and worry. Low tolerance for uncertainty and constant worry can exacerbate stress, ultimately leading to increased blood pressure.
Similarly, depression can directly and indirectly affect hypertension through ambiguity tolerance and worry. Depression can directly elevate blood pressure by creating negative emotions and reducing physical activity. Moreover, depression can indirectly increase blood pressure by heightening worry and lowering ambiguity tolerance. Depressed individuals may experience more worry and less tolerance for ambiguity, both of which contribute to higher blood pressure.
Our study also identified worry and ambiguity tolerance as independent predictors of hypertension. Chronic worry can lead to sustained stress, increasing the risk of hypertension. Individuals with low ambiguity tolerance may experience heightened stress in uncertain situations, further contributing to hypertension. Interestingly, our findings suggest that ambiguity tolerance acts as a mediating variable between worry and hypertension. This implies that worry's impact on blood pressure is partially mitigated by higher ambiguity tolerance. Therefore, improving ambiguity tolerance might be a way to reduce the negative effects of worry on blood pressure.
Conclusion
This study highlights the importance of considering psychological factors and stress management in preventing and controlling hypertension in older adults. Our findings suggest that interventions targeting ambiguity tolerance and worry reduction, alongside traditional blood pressure management strategies, could be effective in lowering blood pressure and improving cardiovascular health. Additionally, these results can inform the development of chronic disease management programs aimed at improving health outcomes and reducing complications associated with hypertension. Future research should explore the effectiveness of interventions designed to improve ambiguity tolerance and manage worry in older adults with hypertension.
Study limitations
This study has some limitations that are important to consider. First, the sample population was restricted to individuals from Khoy city, limiting the generalizability of the findings. To strengthen the generalizability, future
research should replicate this study in other regions of the country with more diverse samples. Additionally, employing a multi-center approach in future studies could enhance the robustness of the results.
Despite these limitations, this study provides valuable insights into the role of psychological factors in hypertension among older adults. Based on these findings, incorporating psychological interventions alongside traditional medical treatments might be beneficial for managing blood pressure and reducing hypertension-related complications. Addressing worry, depression, and their mediating factors could offer a more holistic approach to improving health outcomes in this population.
Conflict of interest
The authors declare no conflicts of interest.
Acknowledgments
We would like to express our sincere gratitude to all the participants who cooperated by completing the questionnaires for this research. Their contribution was essential to this study.
Authors' contributions
All authors significantly contributed to the design and conceptualization of this work. The second author (SA) was responsible for conducting the statistical analysis of the data. The third (KB) and fourth (NA) authors were responsible for drafting the manuscript. All of the authors reviewed the manuscript critically for important intellectual content; and approved the final version to be published; and agreed to be accountable for all aspects of the work.
References
1. Gui J, Li Y, Liu H, Guo L, Li J, Lei Y, et al. Obesity-and lipid-related indices as a risk factor of hypertension in mid-aged and elderly Chinese: a cross-sectional study. BMC Geriatrics. 2024; 24(1): 1-13.
2. Wang S, Shen C, Yang S. Analysis of health-related quality of life in elderly patients with stroke complicated by hypertension in china using the EQ-5D-3L scale. Journal of Multidisciplinary Healthcare. 2024; 17: 1981-97.
3. Jakovljevic M, Westerman R, Sharma T, Lamnisos D. Aging and global health. Handbook of Global Health. 2021: 73-102.
4. Mohammadi S, Hassanipour S, Delam H, Nikbakht HA, Far ZG, Firoozi D, et al. Prevalence of hypertension in Iran: An updated systematic review and meta-analysis of community-based studies. Caspian Journal of Internal Medicine. 2023; 14(4): 607-17.
5. Xu Z, Wu X, Xiao C, Zhang W, Yan P, Yang C, et al. Observational and genetic analyses of the bidirectional relationship between depression and hypertension. Journal of Affective Disorders. 2024; 348: 62-9.
6. Devita M, De Salvo R, Ravelli A, De Rui M, Coin A, Sergi G, et al. Recognizing depression in the elderly: practical guidance and challenges for clinical management. Neuropsychiatric Disease and Treatment. 2022; 18: 2867-80.
7. Pengpid S, Peltzer K. Associations between sensory loss and depressive symptoms in a longitudinal national study of ageing adults in Thailand. Elderly Health Journal. 2023; 9(2): 73-8.
8. Bhat SK, Beilin LJ, Robinson M, Burrows S, Mori TA. Relationships between depression and anxiety symptoms scores and blood pressure in young adults. Journal of Hypertension. 2017; 35(10): 1983-91.
9. Pervichko E, Podstreshnaya A, Koniukhovskaia J. Motivation and perfectionism in middle-age patients with essential hypertension. European Psychiatry. 2020; 63.
10. Rice KG, Suh H, Davis DE. Perfectionism and emotion regulation In Stoeber J, editors. The psychology of perfectionism: Theory, research, applications. Routledge/Taylor & Francis Group; 2017. p. 243-62.
11. Albert P, Rice KG, Caffee L. Perfectionism affects blood pressure in response to repeated exposure to stress. Stress and Health. 2016; 32(2): 157-66.
12. Torres JM, Deardorff J, Holland N, Harley KG, Kogut K, Long K, Eskenazi B. Deportation worry, cardiovascular disease risk factor trajectories, and incident hypertension: A community-based cohort study. Journal of the American Heart Association. 2019; 8(23): 1-10.
13. Ndoja S, Chahine S, Saklofske DH, Lanting B. The erosion of ambiguity tolerance and sustainment of perfectionism in undergraduate medical training: results from multiple samplings of a single cohort. BMC Medical Education. 2020; 20:1-7.
14. Kang W, Pineda Hernández S. Understanding cognitive deficits in people with high blood pressure. Journal of Personalized Medicine. 2023; 13(11): 1-9.
15. Liu S, Yan Y, Gao X, Xiang S, Sha T, Zeng G, et al. Risk factors for postpartum depression among Chinese women: path model analysis. BMC Pregnancy and Childbirth. 2017; 17: 1-7.
16. Fidell LS, Tabachnick BG. Preparatory data analysis. Handbook of psychology: Research Methods in Psychology. 2003; 2: 115-41.
17. Green SB. How many subjects does it take to do a regression analysis. Multivariate Behavioral Research. 1991; 26(3): 499-510.
18. Sisay T, Mulate M, Hailu T, Belete TM. The prevalence of depression and anxiety among cardiovascular patients at University of Gondar specialized hospital using beck's depression inventory II and beck anxiety inventory: A cross-sectional study. Heliyon. 2024; 10(2): 1-9.
19. Segal DL, Coolidge FL, Cahill BS, O'Riley AA. Psychometric properties of the Beck Depression Inventory—II (BDI-II) among community-dwelling older adults. Behavior Modification. 2008; 32(1): 3-20.
20. Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory-Second edition: BDI-II-PERSIAN. Depression and Anxiety. 2005; 21(4): 185-92.
21. Salarifar M, Pouretemad H. P-1060-The study of factorial structure, validity and reliability of the penn state worry questionnaire (PSWQ). European Psychiatry. 2012; 27(S1): 1.
22. Azizi M, Sedaghat Z, Direkvand-Moghadam A. Effect of critical thinking education on problem solving skills and self-esteem in Iranian female students. Journal of Clinical & Diagnostic Research. 2018; 12(1): 1-4.
23. Yaghoobi S, Motevalli M. Structural equations modeling of tendency to critical thinking, problem solving skills and self-esteem among students. International Journal of Medical Investigation. 2020; 9(2): 174-90.
24. Saeedyan M, Mohammadi MA, Mirzaei A, Mozaffari N. Predictors of problem-solving skills among emergency medical services staff in Iran: A cross-sectional correlational study. Frontiers in Psychology. 2022; 13: 1-9.
25. Vahedi VS, Fatemi AH. The role of emotional intelligence and tolerance of ambiguity in academic Iranian EFL learners' willingness to communicate. Journal of Language Teaching and Research. 2016; 7(1): 178-84.
26. Feizi A, Mahbobi T, Zare H, Mostafaei A. The relationship of cognitive intelligence and ambiguity tolerance with entrepreneurship among students of West Azarbayjan Payam Noor University, Iran. Journal of Research in Behavioural Sciences. 2012; 10(4 (25)): 276-84.
27. Aalipour K, Abbasi M, Mirderikvand F. The effect of breath’s thinking strategies training on subjective well-being and tolerance of ambigutiy among female secondary high schools students in Khorramabad city. Education Strategies in Medical Sciences. 2018; 11(1): 1-8. [Persian]
28. Besharat MA. Development and validation of Tehran multidimensional perfectionism scale. Procedia-Social and Behavioral Sciences. 2011; 30: 79-83.
29. Meyers LS, Gamst G, Guarino AJ. Applied multivariate research: Design and interpretation. Sage Publications; 2016.
These results align with previous research by Albert et al., (11) and Bhat et al., (8). Bhat et al., found an inverse relationship between depression and anxiety scores with hypertension in young adults, partially consistent with our findings for depression but not anxiety. In contrast, our study showed a positive association between worry and hypertension. Additionally, our findings support Albert et al.'s observation that high levels of perfectionistic self-criticism are linked to elevated blood pressure.
The significant role of perfectionism in hypertension can be explained by the constant stress and pressure associated with striving for unrealistic standards. This stress can directly elevate blood pressure. Perfectionism also has an indirect effect through its influence on ambiguity tolerance and worry. Low tolerance for uncertainty and constant worry can exacerbate stress, ultimately leading to increased blood pressure.
Similarly, depression can directly and indirectly affect hypertension through ambiguity tolerance and worry. Depression can directly elevate blood pressure by creating negative emotions and reducing physical activity. Moreover, depression can indirectly increase blood pressure by heightening worry and lowering ambiguity tolerance. Depressed individuals may experience more worry and less tolerance for ambiguity, both of which contribute to higher blood pressure.
Our study also identified worry and ambiguity tolerance as independent predictors of hypertension. Chronic worry can lead to sustained stress, increasing the risk of hypertension. Individuals with low ambiguity tolerance may experience heightened stress in uncertain situations, further contributing to hypertension. Interestingly, our findings suggest that ambiguity tolerance acts as a mediating variable between worry and hypertension. This implies that worry's impact on blood pressure is partially mitigated by higher ambiguity tolerance. Therefore, improving ambiguity tolerance might be a way to reduce the negative effects of worry on blood pressure.
Conclusion
This study highlights the importance of considering psychological factors and stress management in preventing and controlling hypertension in older adults. Our findings suggest that interventions targeting ambiguity tolerance and worry reduction, alongside traditional blood pressure management strategies, could be effective in lowering blood pressure and improving cardiovascular health. Additionally, these results can inform the development of chronic disease management programs aimed at improving health outcomes and reducing complications associated with hypertension. Future research should explore the effectiveness of interventions designed to improve ambiguity tolerance and manage worry in older adults with hypertension.
Study limitations
This study has some limitations that are important to consider. First, the sample population was restricted to individuals from Khoy city, limiting the generalizability of the findings. To strengthen the generalizability, future
research should replicate this study in other regions of the country with more diverse samples. Additionally, employing a multi-center approach in future studies could enhance the robustness of the results.
Despite these limitations, this study provides valuable insights into the role of psychological factors in hypertension among older adults. Based on these findings, incorporating psychological interventions alongside traditional medical treatments might be beneficial for managing blood pressure and reducing hypertension-related complications. Addressing worry, depression, and their mediating factors could offer a more holistic approach to improving health outcomes in this population.
Conflict of interest
The authors declare no conflicts of interest.
Acknowledgments
We would like to express our sincere gratitude to all the participants who cooperated by completing the questionnaires for this research. Their contribution was essential to this study.
Authors' contributions
All authors significantly contributed to the design and conceptualization of this work. The second author (SA) was responsible for conducting the statistical analysis of the data. The third (KB) and fourth (NA) authors were responsible for drafting the manuscript. All of the authors reviewed the manuscript critically for important intellectual content; and approved the final version to be published; and agreed to be accountable for all aspects of the work.
References
1. Gui J, Li Y, Liu H, Guo L, Li J, Lei Y, et al. Obesity-and lipid-related indices as a risk factor of hypertension in mid-aged and elderly Chinese: a cross-sectional study. BMC Geriatrics. 2024; 24(1): 1-13.
2. Wang S, Shen C, Yang S. Analysis of health-related quality of life in elderly patients with stroke complicated by hypertension in china using the EQ-5D-3L scale. Journal of Multidisciplinary Healthcare. 2024; 17: 1981-97.
3. Jakovljevic M, Westerman R, Sharma T, Lamnisos D. Aging and global health. Handbook of Global Health. 2021: 73-102.
4. Mohammadi S, Hassanipour S, Delam H, Nikbakht HA, Far ZG, Firoozi D, et al. Prevalence of hypertension in Iran: An updated systematic review and meta-analysis of community-based studies. Caspian Journal of Internal Medicine. 2023; 14(4): 607-17.
5. Xu Z, Wu X, Xiao C, Zhang W, Yan P, Yang C, et al. Observational and genetic analyses of the bidirectional relationship between depression and hypertension. Journal of Affective Disorders. 2024; 348: 62-9.
6. Devita M, De Salvo R, Ravelli A, De Rui M, Coin A, Sergi G, et al. Recognizing depression in the elderly: practical guidance and challenges for clinical management. Neuropsychiatric Disease and Treatment. 2022; 18: 2867-80.
7. Pengpid S, Peltzer K. Associations between sensory loss and depressive symptoms in a longitudinal national study of ageing adults in Thailand. Elderly Health Journal. 2023; 9(2): 73-8.
8. Bhat SK, Beilin LJ, Robinson M, Burrows S, Mori TA. Relationships between depression and anxiety symptoms scores and blood pressure in young adults. Journal of Hypertension. 2017; 35(10): 1983-91.
9. Pervichko E, Podstreshnaya A, Koniukhovskaia J. Motivation and perfectionism in middle-age patients with essential hypertension. European Psychiatry. 2020; 63.
10. Rice KG, Suh H, Davis DE. Perfectionism and emotion regulation In Stoeber J, editors. The psychology of perfectionism: Theory, research, applications. Routledge/Taylor & Francis Group; 2017. p. 243-62.
11. Albert P, Rice KG, Caffee L. Perfectionism affects blood pressure in response to repeated exposure to stress. Stress and Health. 2016; 32(2): 157-66.
12. Torres JM, Deardorff J, Holland N, Harley KG, Kogut K, Long K, Eskenazi B. Deportation worry, cardiovascular disease risk factor trajectories, and incident hypertension: A community-based cohort study. Journal of the American Heart Association. 2019; 8(23): 1-10.
13. Ndoja S, Chahine S, Saklofske DH, Lanting B. The erosion of ambiguity tolerance and sustainment of perfectionism in undergraduate medical training: results from multiple samplings of a single cohort. BMC Medical Education. 2020; 20:1-7.
14. Kang W, Pineda Hernández S. Understanding cognitive deficits in people with high blood pressure. Journal of Personalized Medicine. 2023; 13(11): 1-9.
15. Liu S, Yan Y, Gao X, Xiang S, Sha T, Zeng G, et al. Risk factors for postpartum depression among Chinese women: path model analysis. BMC Pregnancy and Childbirth. 2017; 17: 1-7.
16. Fidell LS, Tabachnick BG. Preparatory data analysis. Handbook of psychology: Research Methods in Psychology. 2003; 2: 115-41.
17. Green SB. How many subjects does it take to do a regression analysis. Multivariate Behavioral Research. 1991; 26(3): 499-510.
18. Sisay T, Mulate M, Hailu T, Belete TM. The prevalence of depression and anxiety among cardiovascular patients at University of Gondar specialized hospital using beck's depression inventory II and beck anxiety inventory: A cross-sectional study. Heliyon. 2024; 10(2): 1-9.
19. Segal DL, Coolidge FL, Cahill BS, O'Riley AA. Psychometric properties of the Beck Depression Inventory—II (BDI-II) among community-dwelling older adults. Behavior Modification. 2008; 32(1): 3-20.
20. Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory-Second edition: BDI-II-PERSIAN. Depression and Anxiety. 2005; 21(4): 185-92.
21. Salarifar M, Pouretemad H. P-1060-The study of factorial structure, validity and reliability of the penn state worry questionnaire (PSWQ). European Psychiatry. 2012; 27(S1): 1.
22. Azizi M, Sedaghat Z, Direkvand-Moghadam A. Effect of critical thinking education on problem solving skills and self-esteem in Iranian female students. Journal of Clinical & Diagnostic Research. 2018; 12(1): 1-4.
23. Yaghoobi S, Motevalli M. Structural equations modeling of tendency to critical thinking, problem solving skills and self-esteem among students. International Journal of Medical Investigation. 2020; 9(2): 174-90.
24. Saeedyan M, Mohammadi MA, Mirzaei A, Mozaffari N. Predictors of problem-solving skills among emergency medical services staff in Iran: A cross-sectional correlational study. Frontiers in Psychology. 2022; 13: 1-9.
25. Vahedi VS, Fatemi AH. The role of emotional intelligence and tolerance of ambiguity in academic Iranian EFL learners' willingness to communicate. Journal of Language Teaching and Research. 2016; 7(1): 178-84.
26. Feizi A, Mahbobi T, Zare H, Mostafaei A. The relationship of cognitive intelligence and ambiguity tolerance with entrepreneurship among students of West Azarbayjan Payam Noor University, Iran. Journal of Research in Behavioural Sciences. 2012; 10(4 (25)): 276-84.
27. Aalipour K, Abbasi M, Mirderikvand F. The effect of breath’s thinking strategies training on subjective well-being and tolerance of ambigutiy among female secondary high schools students in Khorramabad city. Education Strategies in Medical Sciences. 2018; 11(1): 1-8. [Persian]
28. Besharat MA. Development and validation of Tehran multidimensional perfectionism scale. Procedia-Social and Behavioral Sciences. 2011; 30: 79-83.
29. Meyers LS, Gamst G, Guarino AJ. Applied multivariate research: Design and interpretation. Sage Publications; 2016.
Type of Study: Research |
Subject:
Special
Received: 2024/05/11 | Accepted: 2024/06/22 | Published: 2024/06/21
Received: 2024/05/11 | Accepted: 2024/06/22 | Published: 2024/06/21
References
1. Gui J, Li Y, Liu H, Guo L, Li J, Lei Y, et al. Obesity-and lipid-related indices as a risk factor of hypertension in mid-aged and elderly Chinese: a cross-sectional study. BMC Geriatrics. 2024; 24(1): 1-13.
2. Wang S, Shen C, Yang S. Analysis of health-related quality of life in elderly patients with stroke complicated by hypertension in china using the EQ-5D-3L scale. Journal of Multidisciplinary Healthcare. 2024; 17: 1981-97.
3. Jakovljevic M, Westerman R, Sharma T, Lamnisos D. Aging and global health. Handbook of Global Health. 2021: 73-102.
4. Mohammadi S, Hassanipour S, Delam H, Nikbakht HA, Far ZG, Firoozi D, et al. Prevalence of hypertension in Iran: An updated systematic review and meta-analysis of community-based studies. Caspian Journal of Internal Medicine. 2023; 14(4): 607-17.
5. Xu Z, Wu X, Xiao C, Zhang W, Yan P, Yang C, et al. Observational and genetic analyses of the bidirectional relationship between depression and hypertension. Journal of Affective Disorders. 2024; 348: 62-9.
6. Devita M, De Salvo R, Ravelli A, De Rui M, Coin A, Sergi G, et al. Recognizing depression in the elderly: practical guidance and challenges for clinical management. Neuropsychiatric Disease and Treatment. 2022; 18: 2867-80.
7. Pengpid S, Peltzer K. Associations between sensory loss and depressive symptoms in a longitudinal national study of ageing adults in Thailand. Elderly Health Journal. 2023; 9(2): 73-8.
8. Bhat SK, Beilin LJ, Robinson M, Burrows S, Mori TA. Relationships between depression and anxiety symptoms scores and blood pressure in young adults. Journal of Hypertension. 2017; 35(10): 1983-91.
9. Pervichko E, Podstreshnaya A, Koniukhovskaia J. Motivation and perfectionism in middle-age patients with essential hypertension. European Psychiatry. 2020; 63.
10. Rice KG, Suh H, Davis DE. Perfectionism and emotion regulation In Stoeber J, editors. The psychology of perfectionism: Theory, research, applications. Routledge/Taylor & Francis Group; 2017. p. 243-62.
11. Albert P, Rice KG, Caffee L. Perfectionism affects blood pressure in response to repeated exposure to stress. Stress and Health. 2016; 32(2): 157-66.
12. Torres JM, Deardorff J, Holland N, Harley KG, Kogut K, Long K, Eskenazi B. Deportation worry, cardiovascular disease risk factor trajectories, and incident hypertension: A community-based cohort study. Journal of the American Heart Association. 2019; 8(23): 1-10.
13. Ndoja S, Chahine S, Saklofske DH, Lanting B. The erosion of ambiguity tolerance and sustainment of perfectionism in undergraduate medical training: results from multiple samplings of a single cohort. BMC Medical Education. 2020; 20:1-7.
14. Kang W, Pineda Hernández S. Understanding cognitive deficits in people with high blood pressure. Journal of Personalized Medicine. 2023; 13(11): 1-9.
15. Liu S, Yan Y, Gao X, Xiang S, Sha T, Zeng G, et al. Risk factors for postpartum depression among Chinese women: path model analysis. BMC Pregnancy and Childbirth. 2017; 17: 1-7.
16. Fidell LS, Tabachnick BG. Preparatory data analysis. Handbook of psychology: Research Methods in Psychology. 2003; 2: 115-41.
17. Green SB. How many subjects does it take to do a regression analysis. Multivariate Behavioral Research. 1991; 26(3): 499-510.
18. Sisay T, Mulate M, Hailu T, Belete TM. The prevalence of depression and anxiety among cardiovascular patients at University of Gondar specialized hospital using beck's depression inventory II and beck anxiety inventory: A cross-sectional study. Heliyon. 2024; 10(2): 1-9.
19. Segal DL, Coolidge FL, Cahill BS, O'Riley AA. Psychometric properties of the Beck Depression Inventory—II (BDI-II) among community-dwelling older adults. Behavior Modification. 2008; 32(1): 3-20.
20. Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory-Second edition: BDI-II-PERSIAN. Depression and Anxiety. 2005; 21(4): 185-92.
21. Salarifar M, Pouretemad H. P-1060-The study of factorial structure, validity and reliability of the penn state worry questionnaire (PSWQ). European Psychiatry. 2012; 27(S1): 1.
22. Azizi M, Sedaghat Z, Direkvand-Moghadam A. Effect of critical thinking education on problem solving skills and self-esteem in Iranian female students. Journal of Clinical & Diagnostic Research. 2018; 12(1): 1-4.
23. Yaghoobi S, Motevalli M. Structural equations modeling of tendency to critical thinking, problem solving skills and self-esteem among students. International Journal of Medical Investigation. 2020; 9(2): 174-90.
24. Saeedyan M, Mohammadi MA, Mirzaei A, Mozaffari N. Predictors of problem-solving skills among emergency medical services staff in Iran: A cross-sectional correlational study. Frontiers in Psychology. 2022; 13: 1-9.
25. Vahedi VS, Fatemi AH. The role of emotional intelligence and tolerance of ambiguity in academic Iranian EFL learners' willingness to communicate. Journal of Language Teaching and Research. 2016; 7(1): 178-84.
26. Feizi A, Mahbobi T, Zare H, Mostafaei A. The relationship of cognitive intelligence and ambiguity tolerance with entrepreneurship among students of West Azarbayjan Payam Noor University, Iran. Journal of Research in Behavioural Sciences. 2012; 10(4 (25)): 276-84.
27. Aalipour K, Abbasi M, Mirderikvand F. The effect of breath’s thinking strategies training on subjective well-being and tolerance of ambigutiy among female secondary high schools students in Khorramabad city. Education Strategies in Medical Sciences. 2018; 11(1): 1-8. [Persian]
28. Besharat MA. Development and validation of Tehran multidimensional perfectionism scale. Procedia-Social and Behavioral Sciences. 2011; 30: 79-83.
29. Meyers LS, Gamst G, Guarino AJ. Applied multivariate research: Design and interpretation. Sage Publications; 2016.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |